Health
AIDS groups, activists cautious over ‘prevention’ pill
Anti-retroviral drug reduced HIV infections by 44 percent
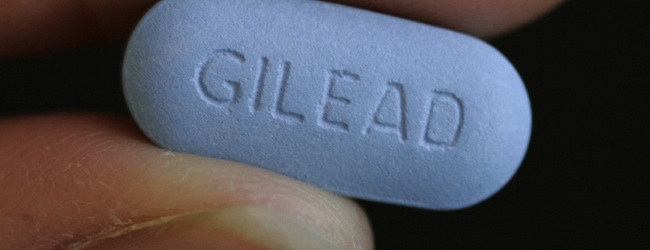
Leaders of AIDS advocacy organizations joined researchers in expressing both optimism and caution over a study released last week showing that the use of a daily anti-retroviral pill significantly lowered the chance of becoming infected by HIV.
The study found that a sample of mostly gay men who were assigned to take a daily tablet of the widely used HIV medication Truvada experienced an average of 43.8 percent fewer HIV infections than participants who received a placebo pill.
Findings of the study were published Nov. 23 in the New England Journal of Medicine.
The study, which began in 2007 and included a total of 2,499 participants in the U.S., Brazil, Ecuador, Peru, South Africa and Thailand, was funded by the National Institutes of Health and the Bill & Melinda Gates Foundation. It was coordinated by the Gladstone Institutes, an arm of the University of California at San Francisco.
Participants were limited to mostly men who have sex with men and a smaller number of transgender women who have sex with men. Researchers conducting the study said the sample was chosen to represent a population group considered at high risk for contracting HIV.
“All study participants received a comprehensive package of prevention services designed to reduce their risk of HIV infection throughout the trial, including HIV testing, intensive safer sex counseling, condoms and treatment and care for sexually transmitted infections,” the Gladstone Institute said in a statement.
NIH official Dr. Anthony Fauci triggered a wave of optimism over the study findings when he told the New York Times last week that the Truvada pill was more than 90 percent effective in preventing HIV infections among a smaller number of study participants who faithfully adhered to the prescribed daily regimen.
The 43.8 percent reduction figure for HIV infections was based on findings from all 1,251 participants who were given the Truvada pill, including many who did not take the daily pill consistently, according to a detailed summary of the study released by the Gladstone Institutes.
The summary says 1,248 participants received a placebo pill as part of what Gladstone officials called a “double blind” study, in which both participants and employees dispensing the pills did not know who received the drug or the placebo.
In addition to interviewing participants to obtain their own accounts of whether they took the pills every day, researchers conducting the study administered regular blood tests of all participants and were able to confirm which ones took the Truvada pill as directed.
Dr. Kenneth Mayor, medical research director of the Fenway Institute in Boston, an HIV treatment facility that was one of two U.S. sites involved in the study, called the findings “a tremendous step forward” in the quest to lower the rate of HIV infection.
“For more than 15 years, the rate of new infections in the U.S. has been stuck at about 56,000 per year,” Mayor said in a statement. “There has been no downward movement in this number, which has meant that we desperately needed a new approach.
“It’s now possible that within the next few years, we can significantly reduce the number of new infections,” he said.
Other AIDS specialists, including Dr. Ray Martins, medical director of D.C.’s Whitman-Walker Clinic, expressed caution over the implications of the study and the widespread use of a prevention pill approach that researchers call “pre-exposure prophylaxis” or “PreP.”
Martins said the average reduction rate in the study for HIV infections of fewer than 44 percent was lower than he expected and shows a tendency of non-compliance by a large percentage of participants.
Similar to other AIDS specialists assessing the study, Martins expressed concern that a lack of adherence to a daily pill regimen of Truvada or other anti-retroviral medications could result in strains of the HIV virus that are resistant to Truvada or other HIV drugs.
The study showed that just a few participants developed resistant viral strains; they were believed to have become infected before they joined the study, with their infections undetectable at the time.
Martins called Truvada “the major backbone to almost all our current HIV regimens” for treating people with HIV and AIDS.
“So if we increase resistance to those meds and people start transmitting more resistant virus, this could be very bad for the HIV community as a whole,” he said. “To me, that was the most worrisome thing.”
He said Whitman-Walker has no immediate plans to dispense Truvada as a prevention pill for D.C.-area residents who might request it. However, he said the Clinic does prescribe Truvada to people who come to the Clinic for “post-exposure prophylaxis” – a short-term drug regimen used for people who seek treatment immediately after engaging in unsafe sex.
“I think more studies have to be done before we would recommend this as a kind of generalized use,” he said.
Martins said the Clinic would welcome the chance to participate in another study that might offer pre-exposure prophylaxis for patients at its sexually transmitted disease clinic program, who are considered to be among the highest risk group for HIV.
Longtime AIDS researcher and physician Dr. Joseph Sonnabend of San Francisco, where the other U.S. site for the prevention pill study was located, said the reduction rate for HIV infections was far too low to make a Truvada prevention pill useful for large populations.
“Daily Truvada reduced new HIV infections by only 44 percent,” he said in a statement. “This is useless, so how on earth can this be construed as a triumph?”
He said the far higher reduction rate for study participants who adhered to the daily pill regimen was meaningless in drawing conclusions for widespread use of a prevention pill “in real world conditions.”
Some AIDS advocacy organizations also expressed concern that the availability of an HIV prevention pill could result in less adherence to condom use and other safer sex practices.
Jose Zuniga, president of the International Association of Physicians in AIDS Care, called the study “an important first step in validating biomedical prevention of HIV in adults.” However, he pointed to a number of potential drawbacks to the use of Truvada as a prophylaxis in addition to the concern over viral resistance to the drug.
Possible side effects to the medication include kidney-related problems with the potential of forcing people to stop taking the medication, Zuniga noted. He said the average cost of $10,000 or more per year for the drug, which likely would not be picked up by health insurance, is also a major concern in considering its widespread use for prevention.
“The bottom line message is that condoms, clean syringes and behavioral interventions must remain our first line of defense against HIV transmission,” Zuniga said.
The study’s organizers at the Gladstone Institutes say the findings show participants increased rather than curtailed safer sex practices during their involvement in the study.
“In fact, self-reported HIV risk behavior decreased among participants in both arms of the study and condom use increased,” Gladstone said in its summary statement.
Among the groups expressing optimism over the study’s findings is Project Inform, a San Francisco-based advocacy organization for the development of effective HIV treatment and prevention options.
“A study showing that a daily pill reduces HIV risk in gay men is reason for great hope,” the group said in a statement. “U.S. agencies should waste no time in assessing the ability of pre-exposure prophylaxis to slow the HIV/AIDS epidemic.”
The group’s four-page analysis of the study is available here.
District of Columbia
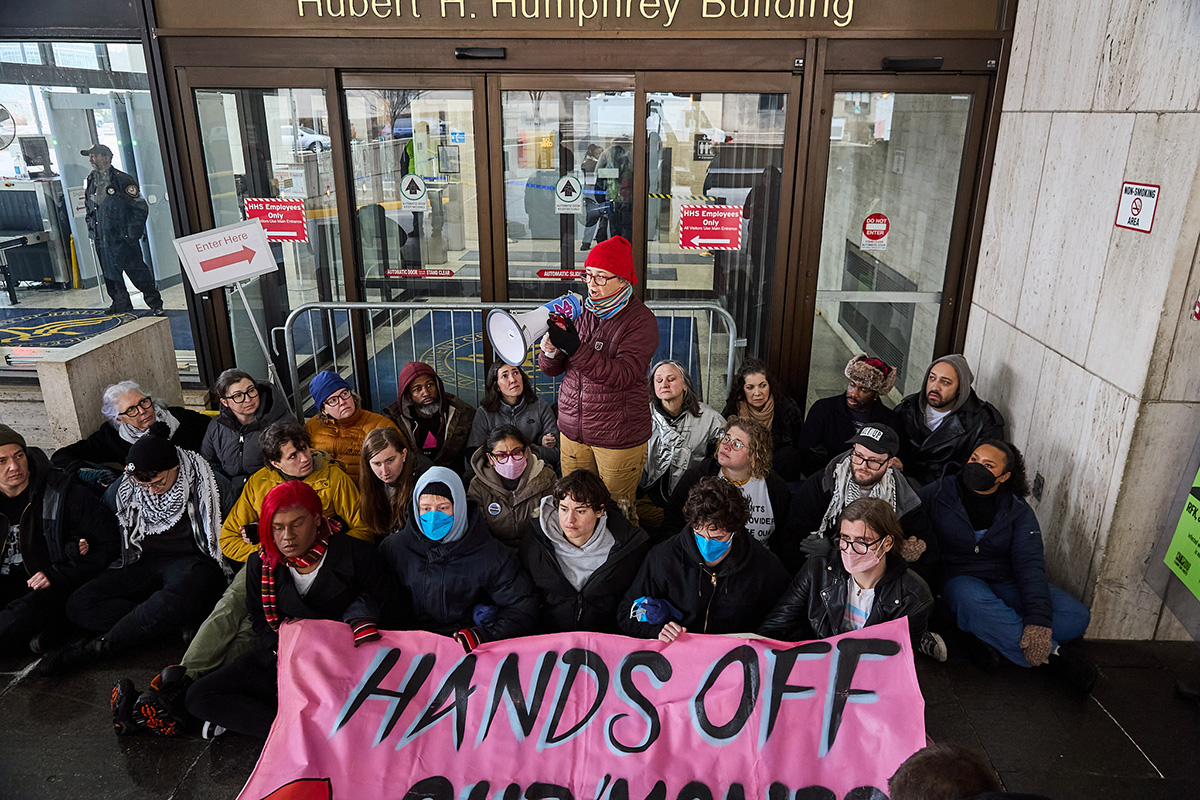
Trans activists arrested outside HHS headquarters in D.C.
Protesters demonstrated directive against gender-affirming care

Authorities on Tuesday arrested 24 activists outside the U.S. Department of Health and Human Services headquarters in D.C.
The Gender Liberation Movement, a national organization that uses direct action, media engagement, and policy advocacy to defend bodily autonomy and self-determination, organized the protest in which more than 50 activists participated. Organizers said the action was a response to changes in federal policy mandated by Executive Order 14187, titled “Protecting Children from Chemical and Surgical Mutilation.”
The order directs federal agencies and programs to work toward “significantly limiting youth access to gender-affirming care nationwide,” according to KFF, a nonpartisan, nonprofit organization that provides independent, fact-based information on national health issues. The executive order also includes claims about gender-affirming care and transgender youth that critics have described as misinformation.
Members of ACT UP NY and ACT UP Pittsburgh also participated in the demonstration, which took place on the final day of the public comment period for proposed federal rules that would restrict access to gender-affirming care.
Demonstrators blocked the building’s main entrance, holding a banner reading “HANDS OFF OUR ‘MONES,” while chanting, “HHS—RFK—TRANS YOUTH ARE NO DEBATE” and “NO HATE—NO FEAR—TRANS YOUTH ARE WELCOME HERE.”
“We want trans youth and their loving families to know that we see them, we cherish them, and we won’t let these attacks go on without a fight,” said GLM co-founder Raquel Willis. “We also want all Americans to understand that Trump, RFK, and their HHS won’t stop at trying to block care for trans youth — they’re coming for trans adults, for those who need treatment from insulin to SSRIs, and all those already failed by a broken health insurance system.”
“It is shameful and intentional that this administration is pitting communities against one another by weaponizing Medicaid funding to strip care from trans youth. This has nothing to do with protecting health and everything to do with political distraction,” added GLM co-founder Eliel Cruz. “They are targeting young people to deflect from their failure to deliver for working families across the country. Instead of restricting care, we should be expanding it. Healthcare is a human right, and it must be accessible to every person — without cost or exception.”
Despite HHS’s efforts to restrict gender-affirming care for trans youth, major medical associations — including the American Medical Association, the American Academy of Pediatrics, and the Endocrine Society — continue to regard such care as evidence-based treatment. Gender-affirming care can include psychotherapy, social support, and, when clinically appropriate, puberty blockers and hormone therapy.
The protest comes amid broader shifts in access to care nationwide.
NYU Langone Health recently announced it will stop providing transition-related medical care to minors and will no longer accept new patients into its Transgender Youth Health Program following President Donald Trump’s January 2025 executive order targeting trans healthcare.
Health
CMS moves to expand HIV-positive organ transplants
HIV/AIDS activists welcome potential development

The Centers for Medicare and Medicaid Services is pushing forward a proposed rule that would make it not only easier for people with HIV in need to get organ transplants from HIV-positive donors, but also make it a priority where there was often a barrier.
The Washington Blade sat down with people familiar with this topic — from former heads of the Centers for Disease Control and Prevention, to HIV activists and to the first HIV-positive person to donate an organ — about what this proposed change could mean.
HIV is a virus that attacks the body’s immune system, particularly targeting the body’s T-cells, which makes it harder to fight off infection and disease. If left untreated, HIV can become AIDS. Without treatment, AIDS can lead to death within a few months or years. The virus is spread through direct contact with bodily fluids — often through sex, unclean needles, or from mother to baby during pregnancy.
According to HIV.gov, a website managed by the U.S. Department of Health and Human Services, approximately 1.2 million people in the U.S. were living with HIV in 2022. Of those 1.2 million, 13 percent don’t know they have it.
The virus disproportionately impacts men who have sex with men and people of color.
The CDC’s statistics show men are most affected, making up almost 80 percent of diagnoses, with gay and bisexual men accounting for the majority. Racial disparities also are present — Black people make up 38 percent of diagnoses. The World Health Organization estimates that around 44.1 million people have died from AIDS-related illnesses globally as of 2024.
Since the virus was first detected 45 years ago, scientists have been working on ways to treat and prevent its spread. In 1987, the first breakthrough in fighting HIV came as the U.S. approved the first HIV medication, AZT — marking the beginning of antiretroviral therapy. This medicine — and later descendants of it, like today’s widely prescribed Biktarvy — stop the HIV virus from reproducing and allow the body to keep its T-cells.
Then in 2012, another big step toward minimizing the scope of the potentially fatal disease came as the CDC approved the first HIV prevention medication, Truvada, more commonly known as PrEP. As of 2024, nearly 600,000 people in the U.S. are using PrEP, according to AIDSVu, which uses data from Gilead Sciences (manufacturers of Truvada and Biktarvy) and is compiled by researchers at the Rollins School of Public Health at Emory University.
The following year, in 2013, the HIV Organ Policy Equity (HOPE) Act was signed into law, enabling the use of organs from HIV-positive donors for transplants into HIV-positive recipients, overturning a 1988 ban.
There are an estimated 123,000 people waiting for organ transplants in the U.S. The number of HIV-positive people on that list is estimated to be smaller, harder to precisely quantify, but they are still in dire need.
A study from the New England Journal of Medicine, published in 2024, analyzed the outcomes of 198 kidney transplantations to people with HIV at 26 medical centers across the U.S. from 2018 to 2021.
Results from the study showed that for kidney transplants performed using organs from 99 donors with HIV and 99 without HIV, one-year survival rates for HIV-positive recipients were nearly identical (94 percent and 95 percent, respectively). Three-year survival rates were also similar (85 percent and 87 percent). Organ rejection rates were also numerically on par after three years (21 percent and 24 percent). Other measures for surgical outcomes, including the number of side effects that occurred, were also roughly the same for both groups.
This shows that, overall, HIV-positive-to-HIV-positive transplants are nearly identical in outcome to transplants between HIV-negative donors and recipients.
Where we are now
Now in 2026, CMS is pushing past the clinical trial testing phase it has been in, making HIV-positive-to-HIV-positive organ transplants more widespread and more accessible.
Adrian Shanker, the former deputy assistant secretary for health policy and senior advisor on LGBTQ health equity at HHS, explained to the Blade that the HOPE Act was a step in the right direction, but this policy change from CMS will expand the ability to help HIV-positive patients in need.
“The original HOPE Act asked for scientific research,” Shanker explained. “There were 10 years of clinical trials. The Biden administration promulgated a rule that removed clinical trial requirements for kidney and liver transplants between people living with HIV. This proposed rule is further implementation on the CMS side with the organ procurement organizations to ensure they’re carrying out the stated intent of the HOPE Act law. It’s building on consensus that has existed through multiple administrations.”
The proposed change would go into effect on July 1, and, according to Shanker, would help everyone in need of an organ — not just HIV-positive people.
“People living with HIV, their ability to receive organs from other people living with HIV in a more streamlined way means that the overall organ waitlist is sped up as well,” he added. “So it benefits everyone on the waitlist.”
Shanker, who was also a member of the Presidential Advisory Council on HIV/AIDS, spoke about how this is a rare moment of bipartisanship.
“There’s no secret that the Trump administration has been quite adversarial to LGBTQI plus health, and to the health of people living with HIV/HIV prevention resources as well … From destabilizing PEPFAR to shutting down one of the primary implementation partners, which is USAID, to firing almost the entire staff of the Office of Infectious Disease and HIV Policy at HHS … But what this is is a glimmer of hope that we can have bipartisan solutions that improve quality of life for people living with HIV.”
Harold Phillips, the CEO of NMAC, a national HIV/AIDS organization that pushes policy education and public engagement to end the HIV epidemic, and an HIV-positive American, sees this as a huge gain for the HIV-positive community.
“For a number of years, we were excluded from that pool of potential donors,” Phillips said. “Many people living with HIV were excluded from being able to get organ transplants. So this opens up that door. This is a positive step forward that will help save lives.”
That “open door,” Phillips said, does more than just provide life-saving organs to people in the most need. It provides a sense of being able to support their community.
“I remember when I was no longer able to check that box on my driver’s license,” Phillips recalled during his interview with the Blade. “I remember what that meant — that my organs might not be able to save a life. The potential that now they could is really exciting for me.”
“To think about people living with HIV donating their organs to other people living with HIV and helping extend their health and well-being — that’s an exciting moment in our history. It reinforces that HIV is not a death sentence anymore.”
Human Rights Campaign Senior Public Policy Advocate Matt Rose also sat down with the Blade to explain the realities of HIV-positive people in the U.S. right now who are looking for a transplant.
“If you’re HIV positive and on the waitlist for an organ right now, your chance of getting one is slim to nil,” Rose said. “This at least gives you a real shot.”
He went on to explain that while the HOPE Act started to move in the right direction, it hasn’t done enough for HIV-positive people in dire need.
“This bill [HOPE] was supposed to fix that — and it never really has. But every administration, we keep chipping away at the next hurdle,” he said. “This latest move will drastically expand the ability for someone who is HIV positive to donate an organ.”
That slow chipping away, in addition to the non-stop trials being done to prove the efficacy and ability for HIV-positive people’s bodies to accept organ donation, is part of the broader push to normalize this practice and remove outdated restrictions.
Shanker elaborated, explaining all that time was necessary to figure out the efficacy of HIV-positive-to-HIV-positive organ transplants but now that the data has been collected — its time to expand the availability.
“There were over a decade of clinical trials between the original HOPE Act law being signed by President Obama and our rule being promulgated at the end of the Biden administration. It was to allow those clinical trials to run their course,” Shanker said.
Nina Martinez is the first HIV-positive person to donate an organ to another person with HIV.
She explained that the stigma and lack of understanding from the general public is another hurdle that those working to improve the quality of life for people living with HIV have to deal with.
“People don’t generally understand that treatment works,” Martinez said, who became the first person to undergo HIV-positive organ donation in 2019. “When you have access to antiretroviral therapy, it lowers the virus in your bloodstream to levels so low that lab tests can’t detect it. Clinically, that correlates to good health and an inability to transmit HIV sexually. I was healthy enough to pass the same evaluation as any other living donor without HIV.”
She continued explaining:
“Just by having a diagnosis of HIV, they’re labeling donors as medically complex, and that’s not accurate. Every donor with HIV has to pass the same evaluation as donors without HIV,” she said. “If someone passes that evaluation and still isn’t allowed to donate, that’s discrimination. If a patient is willing to accept that organ and you block it because of preconceived notions, you’re denying someone care based on disability. That runs counter to basic fairness.”
When asked about her decision to become a donor and what message she hopes it sends, Martinez emphasized that the choice should remain personal.
“I didn’t undertake this endeavor to say that people with HIV should donate. This is a community that’s been through a lot and has contributed to science — we have served. But for people who wanted a way to leave a legacy, and that is what I wanted, they should be supported in that. There shouldn’t be arcane scientific perceptions and myths getting in the way of that.”
National Donor Day, which raises awareness of organ donation, is on Feb. 14. To become an organ donor, visit registerme.org.
Health
CVS Health agrees to cover new HIV prevention drug
‘Groundbreaking’ PrEP medication taken by injection once every six months

CVS Health, the nation’s second largest pharmacy benefit manager company that plays a key role in deciding which drugs are covered by health insurance policies, has belatedly agreed to cover the new highly acclaimed HIV prevention drug yeztugo.
The U.S. Food and Drug Administration approved the use of yeztugo as an HIV prevention or “PrEP” medication in June 2025 as the first such drug to be taken by injection just once every six months. AIDS activists hailed the drug as a major breakthrough in the longstanding effort to end the HIV epidemic.
“We are pleased that CVS Health has finally decided to cover this groundbreaking new PrEP mediation,” said Carl Schmid, executive director of the HIV+ Hepatitis Policy Institute.
“Four months ago, 63 HIV organizations joined us in sending a letter to CVS’s president urging them to reconsider their refusal to cover Yeztugo and reminding them of their legal obligation to cover PrEP and describe the important benefits the drug would bring to preventing HIV in the U.S.,” Schmid said in a statement.
He noted that CVS Health now joins other leading pharmacy benefit manager companies and insurers in covering yeztugo. Gilead Sciences, the pharmaceutical company that developed and manufactures yeztugo, has said 85 percent of all people with health insurance in the U.S. now have coverage for the drug, according to Schmid.
“However, coverage does not automatically translate into access and usage,” Schmid said in his statement. “Too many people are being forced to pay copays while other payers, including employers, are failing to cover all forms of PrEP,” he said.
According to Schmid, the HIV+ Hepatitis Policy Institute is joining other HIV advocacy organizations in urging federal and state government officials to engage in “aggressive enforcement of PrEP insurance coverage requirements and sustained funding of state, local, and community HIV prevention programs.”