Health
AIDS groups, activists cautious over ‘prevention’ pill
Anti-retroviral drug reduced HIV infections by 44 percent
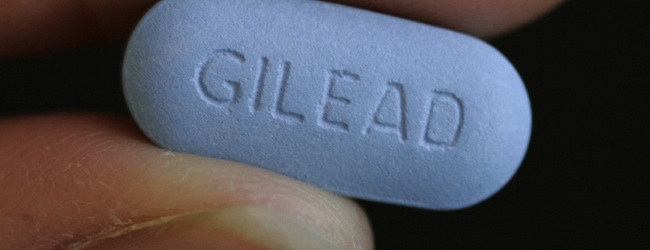
Leaders of AIDS advocacy organizations joined researchers in expressing both optimism and caution over a study released last week showing that the use of a daily anti-retroviral pill significantly lowered the chance of becoming infected by HIV.
The study found that a sample of mostly gay men who were assigned to take a daily tablet of the widely used HIV medication Truvada experienced an average of 43.8 percent fewer HIV infections than participants who received a placebo pill.
Findings of the study were published Nov. 23 in the New England Journal of Medicine.
The study, which began in 2007 and included a total of 2,499 participants in the U.S., Brazil, Ecuador, Peru, South Africa and Thailand, was funded by the National Institutes of Health and the Bill & Melinda Gates Foundation. It was coordinated by the Gladstone Institutes, an arm of the University of California at San Francisco.
Participants were limited to mostly men who have sex with men and a smaller number of transgender women who have sex with men. Researchers conducting the study said the sample was chosen to represent a population group considered at high risk for contracting HIV.
“All study participants received a comprehensive package of prevention services designed to reduce their risk of HIV infection throughout the trial, including HIV testing, intensive safer sex counseling, condoms and treatment and care for sexually transmitted infections,” the Gladstone Institute said in a statement.
NIH official Dr. Anthony Fauci triggered a wave of optimism over the study findings when he told the New York Times last week that the Truvada pill was more than 90 percent effective in preventing HIV infections among a smaller number of study participants who faithfully adhered to the prescribed daily regimen.
The 43.8 percent reduction figure for HIV infections was based on findings from all 1,251 participants who were given the Truvada pill, including many who did not take the daily pill consistently, according to a detailed summary of the study released by the Gladstone Institutes.
The summary says 1,248 participants received a placebo pill as part of what Gladstone officials called a “double blind” study, in which both participants and employees dispensing the pills did not know who received the drug or the placebo.
In addition to interviewing participants to obtain their own accounts of whether they took the pills every day, researchers conducting the study administered regular blood tests of all participants and were able to confirm which ones took the Truvada pill as directed.
Dr. Kenneth Mayor, medical research director of the Fenway Institute in Boston, an HIV treatment facility that was one of two U.S. sites involved in the study, called the findings “a tremendous step forward” in the quest to lower the rate of HIV infection.
“For more than 15 years, the rate of new infections in the U.S. has been stuck at about 56,000 per year,” Mayor said in a statement. “There has been no downward movement in this number, which has meant that we desperately needed a new approach.
“It’s now possible that within the next few years, we can significantly reduce the number of new infections,” he said.
Other AIDS specialists, including Dr. Ray Martins, medical director of D.C.’s Whitman-Walker Clinic, expressed caution over the implications of the study and the widespread use of a prevention pill approach that researchers call “pre-exposure prophylaxis” or “PreP.”
Martins said the average reduction rate in the study for HIV infections of fewer than 44 percent was lower than he expected and shows a tendency of non-compliance by a large percentage of participants.
Similar to other AIDS specialists assessing the study, Martins expressed concern that a lack of adherence to a daily pill regimen of Truvada or other anti-retroviral medications could result in strains of the HIV virus that are resistant to Truvada or other HIV drugs.
The study showed that just a few participants developed resistant viral strains; they were believed to have become infected before they joined the study, with their infections undetectable at the time.
Martins called Truvada “the major backbone to almost all our current HIV regimens” for treating people with HIV and AIDS.
“So if we increase resistance to those meds and people start transmitting more resistant virus, this could be very bad for the HIV community as a whole,” he said. “To me, that was the most worrisome thing.”
He said Whitman-Walker has no immediate plans to dispense Truvada as a prevention pill for D.C.-area residents who might request it. However, he said the Clinic does prescribe Truvada to people who come to the Clinic for “post-exposure prophylaxis” – a short-term drug regimen used for people who seek treatment immediately after engaging in unsafe sex.
“I think more studies have to be done before we would recommend this as a kind of generalized use,” he said.
Martins said the Clinic would welcome the chance to participate in another study that might offer pre-exposure prophylaxis for patients at its sexually transmitted disease clinic program, who are considered to be among the highest risk group for HIV.
Longtime AIDS researcher and physician Dr. Joseph Sonnabend of San Francisco, where the other U.S. site for the prevention pill study was located, said the reduction rate for HIV infections was far too low to make a Truvada prevention pill useful for large populations.
“Daily Truvada reduced new HIV infections by only 44 percent,” he said in a statement. “This is useless, so how on earth can this be construed as a triumph?”
He said the far higher reduction rate for study participants who adhered to the daily pill regimen was meaningless in drawing conclusions for widespread use of a prevention pill “in real world conditions.”
Some AIDS advocacy organizations also expressed concern that the availability of an HIV prevention pill could result in less adherence to condom use and other safer sex practices.
Jose Zuniga, president of the International Association of Physicians in AIDS Care, called the study “an important first step in validating biomedical prevention of HIV in adults.” However, he pointed to a number of potential drawbacks to the use of Truvada as a prophylaxis in addition to the concern over viral resistance to the drug.
Possible side effects to the medication include kidney-related problems with the potential of forcing people to stop taking the medication, Zuniga noted. He said the average cost of $10,000 or more per year for the drug, which likely would not be picked up by health insurance, is also a major concern in considering its widespread use for prevention.
“The bottom line message is that condoms, clean syringes and behavioral interventions must remain our first line of defense against HIV transmission,” Zuniga said.
The study’s organizers at the Gladstone Institutes say the findings show participants increased rather than curtailed safer sex practices during their involvement in the study.
“In fact, self-reported HIV risk behavior decreased among participants in both arms of the study and condom use increased,” Gladstone said in its summary statement.
Among the groups expressing optimism over the study’s findings is Project Inform, a San Francisco-based advocacy organization for the development of effective HIV treatment and prevention options.
“A study showing that a daily pill reduces HIV risk in gay men is reason for great hope,” the group said in a statement. “U.S. agencies should waste no time in assessing the ability of pre-exposure prophylaxis to slow the HIV/AIDS epidemic.”
The group’s four-page analysis of the study is available here.
Health
MISTR announces it’s now prescribing DoxyPE

MISTR, the telemedicine provider that offers free online PrEP and long-term HIV care in all 50 states, D.C., and Puerto Rico, announced it is now prescribing Doxycycline Post-Exposure Prophylaxis (DoxyPEP), an antibiotic that reduces bacterial STIs, including gonorrhea, chlamydia, and syphilis. Patients can now use MISTR’s telehealth platform to receive DoxyPEP online for free, according to a release from the company.
With this launch, MISTR plans to offer patients access to post-exposure care, in addition to its existing preventive and long-term HIV treatment options, which include PrEP and antiretroviral therapy (ART). This comes at a time when the rate of STIs continue to rise. In 2022, more than 2.5 million cases of syphilis, gonorrhea, and chlamydia were reported in the U.S; of that population, gay and bisexual men are disproportionately affected, the company reported.
“Despite an ongoing STI epidemic affecting the LGBTQ+ community, there are few resources available for this underserved, vulnerable community to get the preventative medication they need,” said Tristan Schukraft, CEO and founder of MISTR. “I’m proud that MISTR is democratizing access to PrEP, HIV care, and now DoxyPEP.”
An NIH-funded study published by the New England Journal of Medicine in April 2023 found that doxycycline as post-exposure prophylaxis, now known as DoxyPEP, reduced syphilis by 87%, chlamydia by 88%, and gonorrhea by 55% in individuals taking HIV PrEP, and reduced syphilis by 77%, chlamydia by 74% and gonorrhea by 57% in people living with HIV.
MISTR is a telemedicine platform offering free online access to pre-exposure prophylaxis (PrEP) and long-term HIV care Visit mistr.com for more information.
Health
UNAIDS to commemorate Zero Discrimination Day’s 10th anniversary
UN agency urges global action to protect human rights

As the world marks the 10th anniversary of Zero Discrimination Day; UNAIDS is sounding the alarm on the increasing threats to human rights, calling for renewed efforts to protect the rights of all individuals as a fundamental step towards ensuring health for everyone.
Established by UNAIDS a decade ago, Zero Discrimination Day aims to promote equality and fairness regardless of gender, age, sexuality, ethnicity or HIV status. The progress achieved over the past years is now in jeopardy, however, due to rising attacks on the rights of women, LGBTQ people and other marginalized communities.
UNAIDS Executive Director Winnie Byanyima emphasized the critical link between protecting human rights and safeguarding public health.
“The attacks on rights are a threat to freedom and democracy and are harmful to health,” she said in a press release. “Stigma and discrimination obstruct HIV prevention, testing, treatment and care and hold back progress towards ending AIDS by 2030. It is only by protecting everyone’s rights that we can protect everyone’s health.”
Despite challenges, there has been notable progress.
At the onset of the AIDS pandemic more than 40 years ago, two-thirds of countries criminalized consensual same-sex sexual relations. They are now decriminalized in two-thirds of countries. An additional 38 countries around the world have pledged to end HIV-related stigma and discrimination, contributing to positive changes that include 50 million more girls attending school compared to 2015.
To sustain and enhance these advancements; UNAIDS urges global support for women’s rights movements, LGBTQ rights, racial justice, economic justice, climate justice and peace initiatives. By standing with communities advocating for their rights, the U.N. aims to reinforce the collective effort towards a more inclusive and equitable world.
Zero Discrimination Day is observed on March 1.
Events and activities that will take place around the world throughout the month will serve as reminders of the essential lesson and call to action: Protecting everyone’s health is synonymous with protecting everyone’s rights.
“Through upholding rights for all, we will be able to achieve the Sustainable Development Goals and secure a safer, fairer, kinder and happier world — for everyone,” said Byanyima.
Health
New CDC report finds transgender women at higher risk for HIV
More than 1,600 people in seven cities surveyed

The Centers for Disease Control and Prevention issued a new study report this week that revealed that restricted by employment and housing discrimination and lack of access to needed gender-affirming healthcare for transgender women increasing the risk of contracting HIV.
Researchers reviewed data from a 2019-2020 survey, the National HIV Behavioral Surveillance Among Transgender Women, which found that the demographics of HIV/AIDS have been disproportionally high, especially among Black and Latina trans women, who had experienced employment and housing discrimination coupled with lack of access to gender-affirming healthcare.
The Jan. 25 Morbidity and Mortality Weekly Report was based on data studies of more than 1,600 trans women in seven major urban locales. Participants from Atlanta, Los Angeles, New Orleans, New York, Philadelphia, San Francisco and Seattle were chosen by referrals from people and community-based organizations who knew or were part of the local population of trans women.
The study’s researchers noted: “Employment discrimination occurs at the overlapping nexus of poverty, homelessness, incarceration, health insurance, disability, food insecurity and survival sex work. These issues are interconnected.”
The study stated that trans women’s inability to access quality healthcare, including gender-affirming treatment or access to PrEP, and can expose them to potential incarceration as many turn to “survival sex work” and violence, which increases the risk of contracting HIV.
The study’s author’s pointed out: “When economically marginalized transgender women are refused employment, this refusal cyclically contributes to economic hardships. This analysis …demonstrates the importance of transgender women working and living with dignity and without fear of unfair treatment.”





















