Monkeypox
Monkeypox vaccination effort shifts towards maintaining demand
‘Thousands of shots’ administered at gay events across country
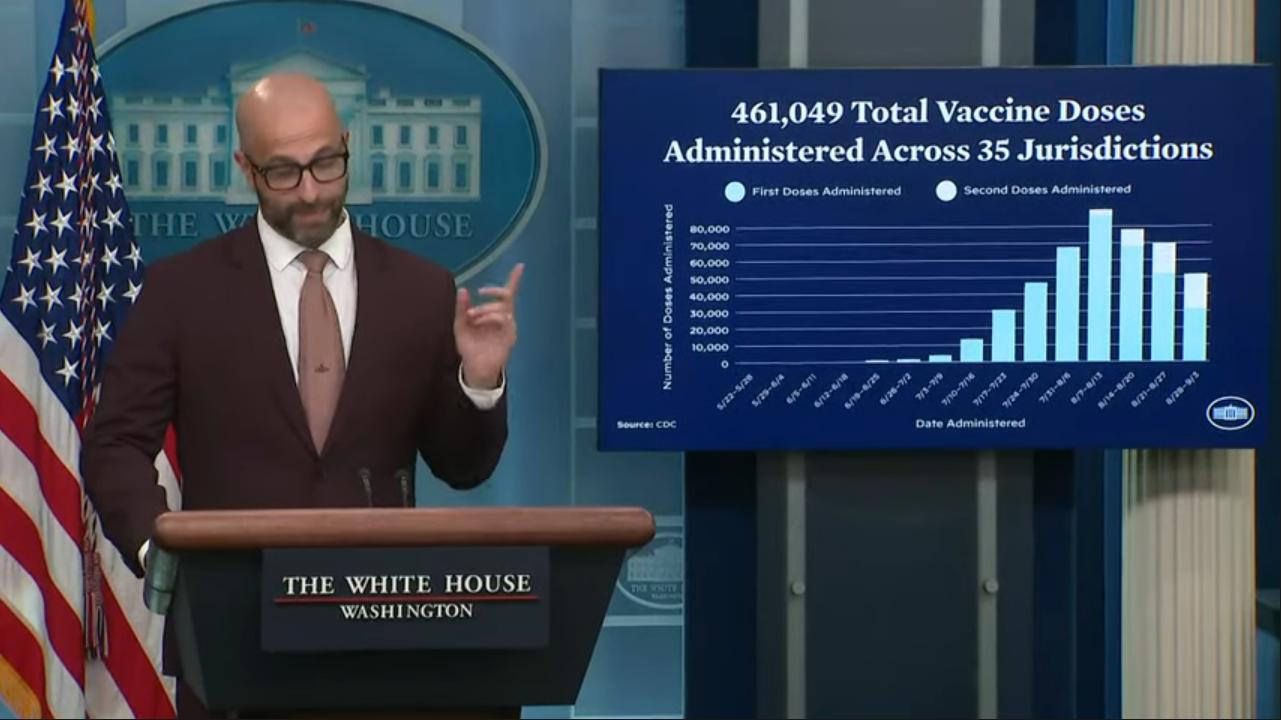
As ensuring adequate supply and distribution of the monkeypox virus vaccine becomes “less of an issue,” efforts have shifted toward maintaining demand, Dr. Demetre Daskalakis, White House national monkeypox response deputy coordinator, said on Sept. 7.
This will mean, “making sure that people know that a effective and safe vaccine is available for those that could benefit,” he said, during a press briefing that also featured National Response Coordinator Dr. Bob Fenton and White House Press Secretary Karine Jean-Pierre.
The officials said they were pleased with the impact of their targeted allocations of vaccine doses to events with large numbers of gay and bisexual men who have sex with men, populations considered high risk for MPV infection.
“Thousands of shots were administered” at Southern Decadence in New Orleans, Black Pride in Atlanta and Oakland Pride in the San Francisco Bay Area, Fenton said. These efforts “were, frankly, wildly successful,” Daskalakis said.
During a Q&A with reporters that followed the briefing, Daskalakis addressed questions about the racial disparities that have begun to emerge with respect to infection and vaccination rates.
According to the Kaiser Family Foundation, “Black people have received 22 percent vaccines, while they account for 36 percent of cases. In contrast, White people have received 63 percent of vaccinations but account for 42 percent of cases.”
Daskalakis explained the events that were targeted this summer were a major part of addressing the disproportionately higher rates of infection and lower rates of vaccination among people of color.
“It’s not about just the vaccine allocation,” he said. “It’s about that intense community engagement that happens on the ground because, ultimately, public health is a local event.”
From the beginning of the outbreak, those engaged in the federal response were in touch with community organizations, Daskalakis said: “Giving the tools that people need to be able to sort of reach health goals is what we’ve been doing. And the support of organizations that serve Black and brown people have been pivotal in really turning the tide in what I think you’re going to see, the new vaccine numbers emerging over the next few weeks.”
Monkeypox
White House monkeypox response coordinator speaks exclusively with Blade
Dr. Demetre Daskalakis joined CDC in late 2020

White House National Monkeypox Response Deputy Coordinator Demetre Daskalakis joined the Los Angeles Blade for an exclusive Zoom interview Wednesday to discuss the latest challenges facing public health officials fighting the monkeypox virus (MPV) – from countering misinformation and educating the public to transitioning to intradermal vaccination dosing regimens.
Daskalakis previously served as medical director for the New York-headquartered Mount Sinai Health System and then was made deputy commissioner for the Division of Disease Control at the New York City Department of Health and Mental Hygiene. In late 2020, as the U.S. saw thousands of new covid fatalities each day, Daskalakis joined the Centers for Disease Control and Prevention’s Division of HIV/AIDS Prevention.
A gay man who is a leading expert on LGBTQ health, during his tenure as a municipal health official in New York, Daskalakis’s work leading HIV and STD health programs was credited with helping to bring down the rate of new HIV infections among the city’s gay and bisexual men by 35 percent.
So, while he notes that the U.S. has never before had a monkeypox outbreak like this one, before he stepped into this role with the White House, Daskalakis’s career had already included significant experience as both a clinical provider and public health official, including work fighting against anti-LGBTQ bias and stigma — which is crucial, given the overrepresentation of MPV cases among men who have sex with men.
When it comes to messaging, Dr. Daskalakis said he and his team have taken the harder but more effective route, which is to center the focus on the means by which one becomes exposed to MPV “and then working really hard to get [messaging] out through the right channels” to the right groups based on their relative risk.
This involves working with a variety of different partners, whether associations of medical providers or groups like the Ryan White HIV/AIDS Program and community-based organizations that serve LGBTQ patients, Daskalakis said. The goal is to “toe the line between making sure you’re giving frank messaging to people while not creating stigma,” he added.
As new data comes in, the communications strategy has shifted accordingly, he said. Such flexibility has become a cornerstone of the coordination of a federal response effort because, “we’ve been able to be way more clear in terms of specific risk factors that potentially increase or decrease an individual’s risk.”
This has meant recommendations that gay and bisexual men “reduce your network of partners and also consider avoiding anonymous sexual partners if you can” are grounded in sound scientific data about the transmissibility of MPV, Daskalakis said.
Another persistent challenge, of course, is the spread of misinformation and disinformation on social media. Last month, extreme right wing U.S. Rep. Marjorie Taylor Greene (R-Ga.) asked on Twitter why children have contracted MPV if the virus is sexually transmitted.
Groups like the Anti-Defamation League cited the move as an example of how “disingenuous questions about the disease’s origin and spread” to draw “an explicit connection between monkeypox and ‘children being molested by homosexuals’” — giving “oxygen and reach” to such dangerous lies about LGBTQ people.
“Stigma is stigma, and homophobia is homophobia,” Daskalakis said, and while these problems are older, more intractable, and broader in scope than public health messaging around MPV, it is important to not “attach an infection to an identity.”
“Stigmatizing a disease and creating stigma really creates rabbit holes that take people away from [figuring out] how to respond to an infectious disease — and the way that you respond to infectious diseases, the focus on community, the focus on knowledge, and the focus on data, which should act as a guidance” in getting messages to people, whether through online social platforms or other channels, he said.
Daskalakis likened the approach to communication around HIV. “Focus on exposure,” he said, explaining that “anal sex is the most common way for HIV to be transmitted” and then making sure that message “goes to people who need to hear it.” That way, men who have sex with men can understand the best harm reduction strategies and “gay sex” or gay and bisexual men are not needlessly linked to the virus in ways that could worsen or intensify stigma.
On Monday, the New York Times reported concerns aired by state and local health officials with the delivery of MPV vaccines, many of whom pointed fingers at their federal counterparts for problems like the arrival of shipments of doses that had been spoiled by high temperatures or improper handling.
Daskalakis acknowledged the challenges while reaffirming the CDC and White House’s commitment to working collaboratively with state and local partners on these efforts.
“The CDC has provided technical assistance, even down to a video that I think actually countries are using now to teach [the proper administration of] intradermal shots, which is really exciting,” he said. “But all of that is really designed to support the jurisdictions and I think we spend our time throughout this entire response really connected with jurisdictions.”
Daskalakis also praised the work being done by local and state health officials: “It’s really important to acknowledge that challenges are real, and [also] the creativity with which they’re sort of addressing those challenges on their jurisdictional level, to really get to the space everyone wants to be, which is more shots in arms … That’s sort of the theme of public health in general, especially in emergency response.” He added that that it’s been encouraging to see “how people are using the guidance of the federal government [including] the support we’re providing, to move things forward.”
Moving forward, notwithstanding the many challenges that lie ahead, Daskalakis is optimistic about the future, partially by virtue of the fact that public health officials will have more data at their disposal. “I think we’re really working to accelerate — with studies that are going to happen — vaccine effectiveness, surveillance and safety that are happening to make sure that we have a sense of how these are working.”
Asked whether the federal coordination efforts remain focused on exploring possible ways to cut through red tape and paperwork, Daskalakis was again positive.
“In terms of bureaucracy, I think that that’s one of the important roles of our coordinating effort,” he said, working with partners at every level to see how the process of vaccinating and treating as many people as possible can be made less burdensome, with less paperwork, and more efficiently.
A promising sign of this kind of breakthrough in the MPV response came last week when the FDA cleared the intradermal injection method of the vaccine JYNNEOS for emergency use authorization.
This route of administration is not only safer, with a superior side effect profile compared to subcutaneous injection, but it also allows for more doses to be administered, Daskalakis said.
In terms of rolling out the intradermal injections of MPV vaccine, Los Angeles is “killing it,” Daskalakis said. “It’s just like lightning speed. It’s inspiring.” It was not easy for such a big city to so quickly adapt to a new method of vaccination, he said, but health officials in the area got creative and “played it right.”
-

 State Department4 days ago
State Department4 days agoState Department releases annual human rights report
-

 District of Columbia2 days ago
District of Columbia2 days agoCatching up with the asexuals and aromantics of D.C.
-

 South America2 days ago
South America2 days agoArgentina government dismisses transgender public sector employees
-

 Maine3 days ago
Maine3 days agoMaine governor signs transgender, abortion sanctuary bill into law












