Health
With time, the Monkeypox vaccine provides good protection
In clinical trials, recipients who were HIV negative had an 83 percent immune response 28 days after one dose compared to 98 percent with two doses at 42 days.

A review of academic literature published in the Journal of Internet Medical Research last year determined, when it comes to information about health topics, social media is not the place to turn. (Unless you follow me, of course!) One study found 87 percent of health-related posts contain misinformation. More than 40 percent of posts about vaccines contain incorrect information.
These findings are, perhaps, not surprising. But they are important to keep in mind as we doom-scroll for information about monkeypox.
I’ve already seen a number of posts on Twitter claiming to have monkeypox breakthrough infections after vaccination. One author said they developed a monkeypox rash two weeks after vaccination. While this person’s experience was not likely a breakthrough case, the post brings up important questions. How much protection does a person have after being vaccinated and when? And, as some cities move to a one-dose regimen due to vaccine supply, what does research say about the number of doses needed to protect a person?
Monkeypox rashes and lesions can take up to three weeks to develop after exposure to the virus, which means it is possible the Twitter user mentioned above was exposed before vaccination or shortly after. The time following vaccination and when you are exposed to the virus matters in terms of the amount of protection you have.
Simply put: vaccines do not offer protection immediately after being administered. Remember what we learned when getting our COVID-19 vaccines: no matter which vaccine you received, you were not fully protected until two weeks after the final dose. For the monkeypox vaccine the time to protection is actually longer. Clinical trials indicated it takes up to four weeks for patients to develop strong protection. In fact, two weeks after the first dose, the immune response was just 29 percent! Take extra care during this period to prevent spread.
Now, what about one dose versus two? With limited monkeypox vaccine supply, cities and states should consider limiting doses to one per person to protect more people.
The U.S. Food and Drug Administration (FDA) approved a vaccine, Jynneos, developed by the U.S. government and Bavarian Nordic in 2019 to protect against both monkeypox and smallpox. The FDA recommended a two dose regimen, four weeks apart. This regimen outperformed an older smallpox vaccine (ACAM2000) for producing an immunological response. The Jynneos vaccine also has fewer side effects and is much safer.
Unfortunately, the Jynneos vaccine is in very short supply. Bavarian Nordic, the only manufacturer of the vaccine worldwide, says it can produce 30 million doses of Jynneos annually, meaning with a full regimen less than 15 million patients worldwide will have full protection. That’s why cities like Washington, D.C. and New York have chosen to move to a single-dose regimen. The United Kingdom and some countries in Europe have done the same.
This approach is the right one.
In clinical trials, recipients who were HIV negative had an 83 percent immune response 28 days after one dose compared to 98 percent with two doses at 42 days. HIV positive recipients had a 67 percent immune response 28 days after one dose. It was 96 percent 42 days after two doses.
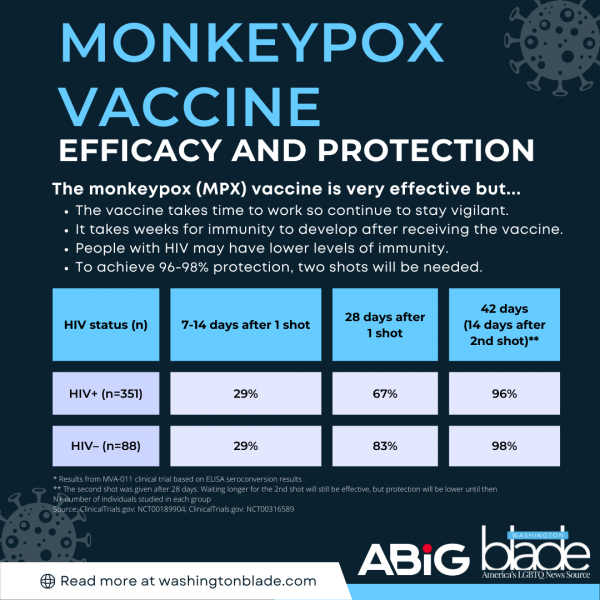
While that data indicates a two-dose regimen is best, with supplies limited, a one-dose regimen for most people is a reasonable approach. That strategy allows double the group of individuals to be immunized — even though there is slightly lower efficacy. A recent article in Science highlighted this important point. Jynneos’ CEO, an immunologist, said one dose of the vaccine conferred a “robust immune response.”
There is one caveat, however. Based on the clinical trial data, we might need to stick with the original two-dose regimen for people who are immunocompromised or live with HIV (irrespective of immune status).
In the face of what appears to be a public health system in disarray, Americans need to be partners in fighting the virus’ spread. Get vaccinated when available. Individuals who are most at risk should sign up now to receive a vaccine. Second, understand it takes time after receiving the vaccine to develop immunity whether you are HIV positive or not. Understand monkeypox symptoms, the timing of symptoms and how to reduce your risk. And, of course, take care when it comes to social media. Spread truth.
Dr. N. Adam Brown is a practicing emergency medicine physician, founder of a healthcare strategy advisory group ABIG Health, and a professor of practice at the University of North Carolina’s Kenan-Flagler Business School. Previously he served as President of Emergency Medicine and Chief Impact Officer for a leading national medical group. Follow him on Twitter @ERDocBrown.
Health
CMS moves to expand HIV-positive organ transplants
HIV/AIDS activists welcome potential development

The Centers for Medicare and Medicaid Services is pushing forward a proposed rule that would make it not only easier for people with HIV in need to get organ transplants from HIV-positive donors, but also make it a priority where there was often a barrier.
The Washington Blade sat down with people familiar with this topic — from former heads of the Centers for Disease Control and Prevention, to HIV activists and to the first HIV-positive person to donate an organ — about what this proposed change could mean.
HIV is a virus that attacks the body’s immune system, particularly targeting the body’s T-cells, which makes it harder to fight off infection and disease. If left untreated, HIV can become AIDS. Without treatment, AIDS can lead to death within a few months or years. The virus is spread through direct contact with bodily fluids — often through sex, unclean needles, or from mother to baby during pregnancy.
According to HIV.gov, a website managed by the U.S. Department of Health and Human Services, approximately 1.2 million people in the U.S. were living with HIV in 2022. Of those 1.2 million, 13 percent don’t know they have it.
The virus disproportionately impacts men who have sex with men and people of color.
The CDC’s statistics show men are most affected, making up almost 80 percent of diagnoses, with gay and bisexual men accounting for the majority. Racial disparities also are present — Black people make up 38 percent of diagnoses. The World Health Organization estimates that around 44.1 million people have died from AIDS-related illnesses globally as of 2024.
Since the virus was first detected 45 years ago, scientists have been working on ways to treat and prevent its spread. In 1987, the first breakthrough in fighting HIV came as the U.S. approved the first HIV medication, AZT — marking the beginning of antiretroviral therapy. This medicine — and later descendants of it, like today’s widely prescribed Biktarvy — stop the HIV virus from reproducing and allow the body to keep its T-cells.
Then in 2012, another big step toward minimizing the scope of the potentially fatal disease came as the CDC approved the first HIV prevention medication, Truvada, more commonly known as PrEP. As of 2024, nearly 600,000 people in the U.S. are using PrEP, according to AIDSVu, which uses data from Gilead Sciences (manufacturers of Truvada and Biktarvy) and is compiled by researchers at the Rollins School of Public Health at Emory University.
The following year, in 2013, the HIV Organ Policy Equity (HOPE) Act was signed into law, enabling the use of organs from HIV-positive donors for transplants into HIV-positive recipients, overturning a 1988 ban.
There are an estimated 123,000 people waiting for organ transplants in the U.S. The number of HIV-positive people on that list is estimated to be smaller, harder to precisely quantify, but they are still in dire need.
A study from the New England Journal of Medicine, published in 2024, analyzed the outcomes of 198 kidney transplantations to people with HIV at 26 medical centers across the U.S. from 2018 to 2021.
Results from the study showed that for kidney transplants performed using organs from 99 donors with HIV and 99 without HIV, one-year survival rates for HIV-positive recipients were nearly identical (94 percent and 95 percent, respectively). Three-year survival rates were also similar (85 percent and 87 percent). Organ rejection rates were also numerically on par after three years (21 percent and 24 percent). Other measures for surgical outcomes, including the number of side effects that occurred, were also roughly the same for both groups.
This shows that, overall, HIV-positive-to-HIV-positive transplants are nearly identical in outcome to transplants between HIV-negative donors and recipients.
Where we are now
Now in 2026, CMS is pushing past the clinical trial testing phase it has been in, making HIV-positive-to-HIV-positive organ transplants more widespread and more accessible.
Adrian Shanker, the former deputy assistant secretary for health policy and senior advisor on LGBTQ health equity at HHS, explained to the Blade that the HOPE Act was a step in the right direction, but this policy change from CMS will expand the ability to help HIV-positive patients in need.
“The original HOPE Act asked for scientific research,” Shanker explained. “There were 10 years of clinical trials. The Biden administration promulgated a rule that removed clinical trial requirements for kidney and liver transplants between people living with HIV. This proposed rule is further implementation on the CMS side with the organ procurement organizations to ensure they’re carrying out the stated intent of the HOPE Act law. It’s building on consensus that has existed through multiple administrations.”
The proposed change would go into effect on July 1, and, according to Shanker, would help everyone in need of an organ — not just HIV-positive people.
“People living with HIV, their ability to receive organs from other people living with HIV in a more streamlined way means that the overall organ waitlist is sped up as well,” he added. “So it benefits everyone on the waitlist.”
Shanker, who was also a member of the Presidential Advisory Council on HIV/AIDS, spoke about how this is a rare moment of bipartisanship.
“There’s no secret that the Trump administration has been quite adversarial to LGBTQI plus health, and to the health of people living with HIV/HIV prevention resources as well … From destabilizing PEPFAR to shutting down one of the primary implementation partners, which is USAID, to firing almost the entire staff of the Office of Infectious Disease and HIV Policy at HHS … But what this is is a glimmer of hope that we can have bipartisan solutions that improve quality of life for people living with HIV.”
Harold Phillips, the CEO of NMAC, a national HIV/AIDS organization that pushes policy education and public engagement to end the HIV epidemic, and an HIV-positive American, sees this as a huge gain for the HIV-positive community.
“For a number of years, we were excluded from that pool of potential donors,” Phillips said. “Many people living with HIV were excluded from being able to get organ transplants. So this opens up that door. This is a positive step forward that will help save lives.”
That “open door,” Phillips said, does more than just provide life-saving organs to people in the most need. It provides a sense of being able to support their community.
“I remember when I was no longer able to check that box on my driver’s license,” Phillips recalled during his interview with the Blade. “I remember what that meant — that my organs might not be able to save a life. The potential that now they could is really exciting for me.”
“To think about people living with HIV donating their organs to other people living with HIV and helping extend their health and well-being — that’s an exciting moment in our history. It reinforces that HIV is not a death sentence anymore.”
Human Rights Campaign Senior Public Policy Advocate Matt Rose also sat down with the Blade to explain the realities of HIV-positive people in the U.S. right now who are looking for a transplant.
“If you’re HIV positive and on the waitlist for an organ right now, your chance of getting one is slim to nil,” Rose said. “This at least gives you a real shot.”
He went on to explain that while the HOPE Act started to move in the right direction, it hasn’t done enough for HIV-positive people in dire need.
“This bill [HOPE] was supposed to fix that — and it never really has. But every administration, we keep chipping away at the next hurdle,” he said. “This latest move will drastically expand the ability for someone who is HIV positive to donate an organ.”
That slow chipping away, in addition to the non-stop trials being done to prove the efficacy and ability for HIV-positive people’s bodies to accept organ donation, is part of the broader push to normalize this practice and remove outdated restrictions.
Shanker elaborated, explaining all that time was necessary to figure out the efficacy of HIV-positive-to-HIV-positive organ transplants but now that the data has been collected — its time to expand the availability.
“There were over a decade of clinical trials between the original HOPE Act law being signed by President Obama and our rule being promulgated at the end of the Biden administration. It was to allow those clinical trials to run their course,” Shanker said.
Nina Martinez is the first HIV-positive person to donate an organ to another person with HIV.
She explained that the stigma and lack of understanding from the general public is another hurdle that those working to improve the quality of life for people living with HIV have to deal with.
“People don’t generally understand that treatment works,” Martinez said, who became the first person to undergo HIV-positive organ donation in 2019. “When you have access to antiretroviral therapy, it lowers the virus in your bloodstream to levels so low that lab tests can’t detect it. Clinically, that correlates to good health and an inability to transmit HIV sexually. I was healthy enough to pass the same evaluation as any other living donor without HIV.”
She continued explaining:
“Just by having a diagnosis of HIV, they’re labeling donors as medically complex, and that’s not accurate. Every donor with HIV has to pass the same evaluation as donors without HIV,” she said. “If someone passes that evaluation and still isn’t allowed to donate, that’s discrimination. If a patient is willing to accept that organ and you block it because of preconceived notions, you’re denying someone care based on disability. That runs counter to basic fairness.”
When asked about her decision to become a donor and what message she hopes it sends, Martinez emphasized that the choice should remain personal.
“I didn’t undertake this endeavor to say that people with HIV should donate. This is a community that’s been through a lot and has contributed to science — we have served. But for people who wanted a way to leave a legacy, and that is what I wanted, they should be supported in that. There shouldn’t be arcane scientific perceptions and myths getting in the way of that.”
National Donor Day, which raises awareness of organ donation, is on Feb. 14. To become an organ donor, visit registerme.org.
Health
CVS Health agrees to cover new HIV prevention drug
‘Groundbreaking’ PrEP medication taken by injection once every six months

CVS Health, the nation’s second largest pharmacy benefit manager company that plays a key role in deciding which drugs are covered by health insurance policies, has belatedly agreed to cover the new highly acclaimed HIV prevention drug yeztugo.
The U.S. Food and Drug Administration approved the use of yeztugo as an HIV prevention or “PrEP” medication in June 2025 as the first such drug to be taken by injection just once every six months. AIDS activists hailed the drug as a major breakthrough in the longstanding effort to end the HIV epidemic.
“We are pleased that CVS Health has finally decided to cover this groundbreaking new PrEP mediation,” said Carl Schmid, executive director of the HIV+ Hepatitis Policy Institute.
“Four months ago, 63 HIV organizations joined us in sending a letter to CVS’s president urging them to reconsider their refusal to cover Yeztugo and reminding them of their legal obligation to cover PrEP and describe the important benefits the drug would bring to preventing HIV in the U.S.,” Schmid said in a statement.
He noted that CVS Health now joins other leading pharmacy benefit manager companies and insurers in covering yeztugo. Gilead Sciences, the pharmaceutical company that developed and manufactures yeztugo, has said 85 percent of all people with health insurance in the U.S. now have coverage for the drug, according to Schmid.
“However, coverage does not automatically translate into access and usage,” Schmid said in his statement. “Too many people are being forced to pay copays while other payers, including employers, are failing to cover all forms of PrEP,” he said.
According to Schmid, the HIV+ Hepatitis Policy Institute is joining other HIV advocacy organizations in urging federal and state government officials to engage in “aggressive enforcement of PrEP insurance coverage requirements and sustained funding of state, local, and community HIV prevention programs.”
Health
Choose U ambassadors share lived experiences with HIV, personal reflections, and insights
The Choose U World AIDS Day panel brought together three longtime advocates living with HIV to talk about care, stigma, and what living with HIV over the long-term means to them. The conversation featured Jahlove Serrano, Joyce Belton, and Andrew Nichols, who have each lived with HIV for more than 20 years. News is Out hosted the event in partnership with Gilead Sciences.
“Co-created with community representatives from around the world, Choose U is comprised of inspiring examples of how the outlook for aging with HIV has dramatically changed,” Gilead shared in the recent launch of the program. “By focusing on the real-world experiences of people in different circumstances, Choose U spotlights individuals prioritizing starting and staying on HIV treatment, self-care, and overall strategies to help them lead healthier lives.”
The Choose U ambassadors opened with a clear message: Lived experience drives understanding.
Each panelist talked through the decisions, relationships, and periods of uncertainty that shaped their HIV care. They also described their approaches to HIV treatment and adherence, including the importance of staying on treatment to help lower the risk of HIV drug resistance. They reflected on the shifts they have seen in HIV treatment over the decades, the value of honest conversations with providers, and how staying engaged in care and on HIV treatment helped them lead longer, healthier lives.
The panel discussed U=U, which stands for “Undetectable equals Untransmittable.” Undetectable means there is so little virus in the blood that a lab test can’t measure it. Research shows that taking HIV treatment as prescribed, and getting to and staying undetectable, prevents HIV from spreading through sex.
The panelists also spoke about the emotional side of living with HIV over the long-term and the stigma they have faced. Joyce described a personal moment when her pastor visited her in the hospital and how that experience began her work educating her church community about HIV.
Jahlove talked about how his biological family reacted to his diagnosis. “When I disclosed my status, they told me that I put a shame on the family,” said Jahlove. When he shared his status with his peers, they responded with support, which gave him a sense of empowerment.
Andrew, a professional therapist, described how he has experienced stigma in dating and in his workplace, and why he turns to therapy for guidance. “Therapy has really helped me rebuild my confidence and realize my self-worth has to come from me,” said Andrew. “Then after that, I can help with the greater community.”
The panel closed with a message for others living with HIV: They encouraged viewers to start and stay engaged in HIV treatment and care, ask questions, and rely on supportive networks. Their stories show how starting and staying on treatment over the long-term, community, and affirmation can shape well-being.
A recording of the full 30-minute event is now available on YouTube, which you can access here.
-

 Baltimore3 days ago
Baltimore3 days ago‘Heated Rivalry’ fandom exposes LGBTQ divide in Baltimore
-

 Real Estate3 days ago
Real Estate3 days agoHome is where the heart is
-

 District of Columbia3 days ago
District of Columbia3 days agoDeon Jones speaks about D.C. Department of Corrections bias lawsuit settlement
-

 European Union3 days ago
European Union3 days agoEuropean Parliament resolution backs ‘full recognition of trans women as women’