National
HIV research sped development of COVID vaccine
Top NIH official says success in coronavirus will boost AIDS work

Since 1996, Carl W. Dieffenbach, who holds a Ph.D. in biophysics from John Hopkins University, has served as director of the Division of AIDS at the National Institute of Allergies and Infectious Diseases, which is an arm of the U.S. National Institutes of Health or NIH.
In a June 10 interview with the Washington Blade, Dieffenbach gave an update on the extensive, ongoing research into the development of an HIV/AIDS vaccine that he has helped to coordinate for many years, including current human trials for a prospective AIDS vaccine taking place in the U.S., South America, and Africa.
One thing he feels passionate about is a development not widely reported in the media reports about the successful development of the COVID-19 vaccine. According to Dieffenbach, the extensive research into an AIDS vaccine in recent and past years, while not yet successful in yielding an effective AIDS vaccine, helped lay the groundwork for the rapid development of the different versions of a COVID vaccine.
“Because my division runs the largest clinical trials program in the word, we jumped in with both feet to help with coronavirus disease for both vaccines and drugs and things like that,” he said. “And the platforms that were used – the way they are making the coronavirus vaccines – the RNA vaccines with Moderna – were first piloted by NIH and Moderna to try to make an HIV vaccine,” Dieffenbach says.
“So, in many ways, the work for the past 25 years that we’ve done in HIV vaccines sped the development of coronavirus vaccines,” he told the Blade. “And now it’s time to take what we’ve learned from coronavirus and take it back to HIV and start afresh or continue with what we have and build upon from what we have learned.”
Dieffenbach says one reason the development of a COVID vaccine came about before an AIDS vaccine, despite more than 20 years of AIDS vaccine research, is that the HIV virus is far more complex than the coronavirus, especially its ability to infect and remain embedded in the infected person for life.
“Back in 2007 we had the first hint that an AIDS vaccine might be possible with a study called RV144,” Dieffenbach says. “We spent 10 years trying to replicate that, and we just completed that study – a study called HVTN702. And it showed no efficacy,” he said, meaning it did not work.
“So that was a big disappointment to us,” he says “But in the meantime, we had pushed forward with the J&J [Johnson and Johnson pharmaceutical company] vaccine and are pretty far along. We’ll see what happens. We should know in the next several months whether the N26 version of an AIDS vaccine, and HIV vaccine works or not,” he says. “We’re very close to an answer.”
Washington Blade: Where do things stand in the development of an HIV/AIDS vaccine in light of Dr. Fauci’s statement a few weeks ago that the development of a COVID-19 vaccine could provide a boost to developing an AIDS vaccine?
Carl Dieffenbach: Sure. So, maybe I can start by introducing myself to you as a way of putting this into a context.
So, I’m the director of the Division of AIDS, which is the largest funder of HIV research in the world. And I report directly to Dr. Fauci. So, I’m responsible for all AIDS, all the time. And that is my passion and purpose in life. Part of that is working toward a safe, effective, and durable HIV vaccine, which has been one of the two most challenging questions left in science today. The other is a cure. They are connected in some ways.
So, with that as background, when coronavirus disease came along – because my division runs the largest clinical trials program in the world – we jumped in with both feet to help with coronavirus disease for both vaccines and drugs and things like that. And the platforms that were used – the way they are making the coronavirus vaccines – the RNA vaccines with Moderna were first piloted by NIH and Moderna to try to make an HIV vaccine. So, we’ve being working on that platform with Moderna for several years.
The leadership at Pfizer used to be part of a group at Penn, where we were also working with them. The J&J vaccine – we currently have in two Phase III clinical trials for HIV, one in sub-Saharan Africa, specifically in young women and the other one in the Americas in men who have sex with men and transgender individuals. Both of those Phase IIIs are moving along. The women’s study is fully enrolled. The men’s study was hit hard by COVID, but we worked through and will be fully enrolled by September.
One other vaccine just to talk about is the Oxford vaccine, the AstraZeneca vaccine. That is also using a platform at Oxford University, which has been used for HIV. So, in many ways, the work for the past 25 years that we’ve done in HIV vaccines sped the development of coronavirus vaccines. And now it’s time to take what we’ve learned from coronavirus and take it back to HIV and start afresh or continue with what we have and build upon from where we have learned.
Blade: That’s very interesting. But can we assume, then, from the clinical trials that have taken place for an HIV vaccine that they did not succeed in providing the immunity needed for an effective vaccine?
Dieffenbach: So, that’s exactly the problem we have. Back in 2007 we had the first hint that an AIDS vaccine might be possible with a study called RV144. We spent 10 years trying to replicate that, and we just completed that study – a study called HVTN702. And it showed no efficacy. So, that was a big disappointment to us. But in the meantime, we had pushed forward with the J&J vaccine and are pretty far along. We’ll see what happens. We should know in the next several months whether the N26 version of an AIDS vaccine, and HIV vaccine works or not. We’re very close to an answer.
Blade: So, the human trials are ongoing.
Dieffenbach: Oh, again – the study in young women in sub-Sahara Africa is fully enrolled. The men’s study will be fully enrolled in September. So, we have fought through the coronavirus epidemic to maintain, to nurse these trials along to make sure with the $100 million or so we’ve invested, that we didn’t want them to go down the drain literally because we lost too many people for follow-up. So, this was a herculean effort that has gone on all the time trying to do the vaccine studies for coronavirus disease, which we were also incredibly successful in.
Blade: Can we assume all of the people participating in the studies were HIV negative?
Dieffenbach: Yes, they’re HIV negative. They are people who are at risk. And also, in South America, for example, the major countries we’re in are Peru and Brazil. And they’ve had a strong research culture with us, going back more than a decade. For example, both of those countries played big roles in our studies of pre-exposure prophylaxis. A study called I-PREX that demonstrated that in men who have sex with men that [a PrEP drug] works well to prevent HIV acquisition in seronegative men who have sex with men.
So, we’ve been there. This is a really good setup for the countries, for the citizens that are in those countries that want to avail themselves to the research that has benefited everybody.
Blade: Among those who are participating in these ongoing AIDS vaccine trials, can we assume they cannot be taking the PrEP anti-retroviral drugs that have been shown to be highly effective in preventing HIV infection?
Dieffenbach: So, what we’ve done is we – everything is by conversation. So, when somebody who is interested in the study comes in, we talk to them. What is your chief interest in being in this study? And a lot of people want to be in the study because then they can access PrEP. They want to make it easier to get a hold of pre-exposure prophylaxis. They feel that is the best way that they can protect themselves.
So, in that situation, what we do is we take those people and link them to PrEP services where they can easily get PrEP in their community. So, first it’s taking care of those people. Then there are people who really have no interest in PrEP. And we actually counsel them every time they come in for a study. Are you sure you don’t want to access PrEP? And those are the people we then say, if you’re not interested in PrEP, what do you think about participating in a vaccine trial?
Because they’re the ones who have the most freedom of thought. They don’t have an opinion about the vaccine or about PrEP. So, those are the people we’ve been focusing on and enrolling. So, we’ve been very careful to make sure that if people wanted PrEP they not only have access, but they didn’t feel like somehow having to trade something in order to get it. The freedom to join a study should be a free choice. And it shouldn’t be a coercive thing to get PrEP. So, we just took that off the table and said if you’re truly interested in PrEP we can get you PrEP and make sure that was available.
Blade: So, in that case, if they choose PrEP they would not be in the vaccine trial?
Dieffenbach: You know, it’s interesting that you ask it in that way. Because you have relationships with your community, many of the investigators have reported that people will say, you know I tried PrEP and it wasn’t for me. It made me gaseous. It upset my stomach. I wasn’t myself. I tried it. I couldn’t make it work for me. I want to stop PrEP. Am I still eligible for the [vaccine] study? And the answer is of course. Many people are very happy on PrEP and they come in for visits occasionally and say this is working for me and just have the relationship with the doctors there, so it works. So, again, it’s about maintaining contact with your communities.
Blade: Can you tell a little about what happens next after people become part of an HIV vaccine trial. Do you have to keep in touch with these people, and do they have to get an HIV test periodically?
Dieffenbach: Exactly. So, the vaccine consists of a series of injections. It’s a mixture of vector systems that delivers a series of encoded HIV genes that are specifically designed to induce very broad immunity. There’s a whole computer-based process to design those components of the vaccine to make sure that it has sequence similarities with all the different versions of HIV circulating in the globe. And then at the end there is a protein boost. And we carry this out.
So, about every three to four months people come in. They get a shot. They fill out questionnaires. They give a blood sample. And they’re tested for HIV and are given a boost or a placebo. And they stay in touch with the clinic. They come in and out of the clinic. And the retention is quite high in these situations because people really like having the attention of the clinic available to them. It’s part of the community.
Blade: So, they go to a clinic for all of this?
Dieffenbach: It’s a research clinic. It’s not like a state-run health clinic. It’s a research clinic. Clinic is just a term for where people are seen.
Blade: Are any of these AIDS vaccine trials that are going on taking place in the United States?
Dieffenbach: Yes. So, the study is called Mosaico. And it’s HVTN706. And we have sites throughout the United States as well as South America. But that study is limited to men who have sex with men – the one in the United States.
Blade: Is it broader than just men who have sex with men in other countries?
Dieffenbach: No, so we decided to really focus on specific at-risk populations. So, in the Americas we chose to focus on men who have sex with men and transgender individuals. And sub-Saharan Africa we focused on young women because that is the target of the study population. So, 705 is all women in sub-Saharan Africa. And in the Americas in North and South America it is all men who have sex with men and transgender individuals.
Blade: Can we assume that the researchers that are doing these studies have a sensitivity of LGBTQ people? Is there still an issue where people worry about being outed as being gay or transgender?
Dieffenbach: So, many of the sites that we work with have been part of our system for over 20 years. And so, they are trusted members of the LGBTQ community within their cities and states. And ‘states’ is a literal term where it’s a state in Colombia or Peru or Brazil. And so, it is part of the fabric of the gay community in these places. Just like in San Francisco the San Francisco health clinic and the DCF clinics are part and parcel of everything the community does there.
And so, the lead physician in San Francisco is Susan Buchbinder. She has been a leader in health in this population for over 25 years or actually closer to 30 years at this point. We’re all getting old. Do you know that? So, we have been at this a very long time. And really have tried to build structures that are durable and therefore are reliable to the community. And that’s where we go back to the same groups time after time.
Blade: Have the locations of the vaccine testing sites been released publicly?
Dieffenbach: Yes, all of that is publicly available on clinicaltrials.gov. If you go into clinicaltrials.gov and search HVTN705 or HVTN706 you will get a version of the protocol, all the times it’s been modified, where we are – the protocol. All of that is public knowledge and available to you. HVTN705 is the women’s study. HVTN706 is the men’s study.
Blade: Is there a timeframe for when these latest vaccine studies might be completed?
Dieffenbach: I think within the next several months. We will get an answer out of the women’s study and then the men’s study is probably a year away. We were slowed a little bit because of COVID. We actually had to pause enrollment for several months. But we’re back on track.
Blade: Isn’t there a parallel research effort for an HIV/AIDS cure?
Dieffenbach: Yes, we have a very large program in cure research. It is a lot earlier in the discovery process and so it’s still very ‘researchy.’ And we have a very large program called the Martin Delany Collaboratories for Cure Research. Martin Delany was an activist who really pushed NIH in so many wonderful ways to really take the need for a cure seriously. His argument was a cure is the next logical step after effective anti-retroviral therapy. You cannot stop with one pill once a day. You’ve got to keep going. And he was pretty persistent. And unfortunately, he died several years go and we just thought the best way to honor him, and his memory was to name a program after him.
Editor’s note: Next week, in the second and final installment of his interview with the Blade, Dr. Dieffenbach discusses the progress in research and studies into an HIV/AIDS cure and explains from a scientific standpoint why an HIV vaccine is taking longer to develop than a COVID vaccine.
Federal Government
Two very different views of the State of the Union
As Trump delivered his SOTU address inside the Capitol, Democratic lawmakers gathered outside in protest, condemning the administration’s harmful policies.

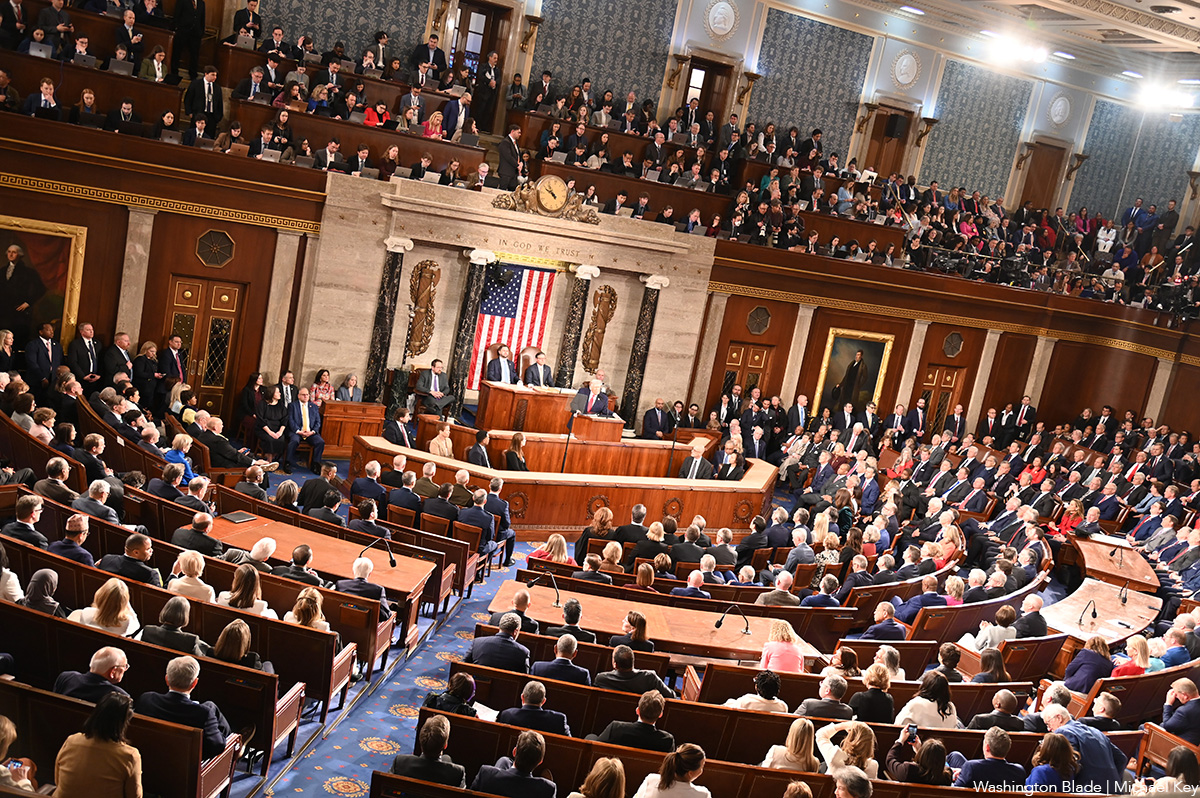
As President Donald Trump delivered his State of the Union address inside the U.S. Capitol — touting his achievements and targeting political enemies — progressive members of Congress gathered just outside in protest.
Their message was blunt: For many Americans, particularly LGBTQ people, the country is not better off.
Each year, as required by Article II, Section 3 of the Constitution, the president must “give to the Congress Information of the State of the Union.” The annual address is meant to outline accomplishments and preview the year ahead. This year, Trump delivered the longest State of the Union in U.S. history, clocking in at one hour and 48 minutes. He spoke about immigration, his “law and order” domestic agenda, his “peace through strength” foreign policy doctrine, and what he framed as the left’s ‘culture wars’ — especially those involving transgender youth and Christian values.
But one year into what he has called the “Trump 2.0” era, the picture painted outside the Capitol stood in stark contrast to the one described inside.
Transgender youth
In one of the most pointed moments of his speech, Trump spotlighted Sage Blair, using her story to portray gender-affirming care as coercive and dangerous. Framing the issue as one of parental rights and government overreach, he told lawmakers and viewers:
“In the gallery tonight are Sage Blair and her mother, Michelle. In 2021, Sage was 14 when school officials in Virginia sought to socially transition her to a new gender, treating her as a boy and hiding it from her parents. Hard to believe, isn’t it? Before long, a confused Sage ran away from home.
“After she was found in a horrific situation in Maryland, a left-wing judge refused to return Sage to her parents because they did not immediately state that their daughter was their son. Sage was thrown into an all-boys state home and suffered terribly for a long time. But today, all of that is behind them because Sage is a proud and wonderful young woman with a full ride scholarship to Liberty University.
“Sage and Michelle, please stand up. And thank you for your great bravery and who can believe that we’re even speaking about things like this. Fifteen years ago, if somebody was up here and said that, they’d say, what’s wrong with him? But now we have to say it because it’s going on all over, numerous states, without even telling the parents.
“But surely, we can all agree no state can be allowed to rip children from their parents’ arms and transition them to a new gender against the parents’ will. Who would believe that we’ve been talking about that? We must ban it and we must ban it immediately. Look, nobody stands up. These people are crazy. I’m telling you, they’re crazy.”
The story, presented as encapsulation of a national crisis, became the foundation for Trump’s renewed call to ban gender-affirming care. LGBTQ advocates — and those familiar with Blair’s story — argue that the situation was far more complex than described and that using a single anecdote to justify sweeping federal restrictions places transgender people, particularly youth, at greater risk.
Equality Virginia said the president’s remarks were part of a broader effort to strip transgender Americans of access to care. In a statement to the Blade, the group said:
“Tonight, the president is choosing to double down on efforts to disrupt access to evidence-based, lifesaving care.
“Rather than allowing families and doctors to navigate deeply personal medical decisions free from federal interference — or allowing schools to respond with nuance and compassion without putting marginalized children at risk — the president is instead advocating for reckless, one-size-fits-all political control.
“At a time when Virginians are worried about rising costs, economic uncertainty, and aggressive immigration enforcement actions disrupting communities and families, attacking transgender young people is a blatant political distraction from the real challenges facing our nation. Virginia families and health care providers do not need Donald Trump telling them what care they do or do not need.”
For many in the LGBTQ community, the rhetoric inside the chamber echoed actions already taken by the administration.
Earlier this month, the Pride flag was removed from the Stonewall National Monument under a National Park Service directive that came from the top. Community members returned to the site, raised the flag again, and filed suit, arguing the removal violated federal law. To advocates, the move was symbolic — a signal that even the legacy of LGBTQ resistance was not immune.
Immigration and fear
Immigration dominated both events as well.
Inside the chamber, Trump boasted about the hundreds of thousands of immigrants detained in makeshift facilities. Outside, Democratic lawmakers described those same facilities as concentration camps and detailed what they characterized as the human toll of the administration’s enforcement policies.
Sen. Ed Markey (D-Mass.), speaking to the crowd, painted a grim picture of communities living in fear:
“People are vanishing into thin air. Quiet mornings are punctuated by jarring violence. Students are assaulted by ICE agents sitting outside the high school, hard working residents are torn from their vehicles in front of their children. Families, hopelessly search for signs of their loved ones who have stopped answering their phones, stop replying to text… This is un-American, it is illegal, it is unconstitutional, and the people are going to rise up and fight for Gladys Vega and all of those poor people who today need to know that the people’s State of the Union is the beginning of a long fight that is going to result in the end of Republican control of the House of Representatives and the Senate in the United States of America in 2026.”
Speakers emphasized that LGBTQ immigrants are often especially vulnerable — fleeing persecution abroad only to face detention and uncertainty in the United States. For them, the immigration crackdown and the attacks on transgender health care are not separate battles but intertwined fronts in a broader cultural and political war.
Queer leadership
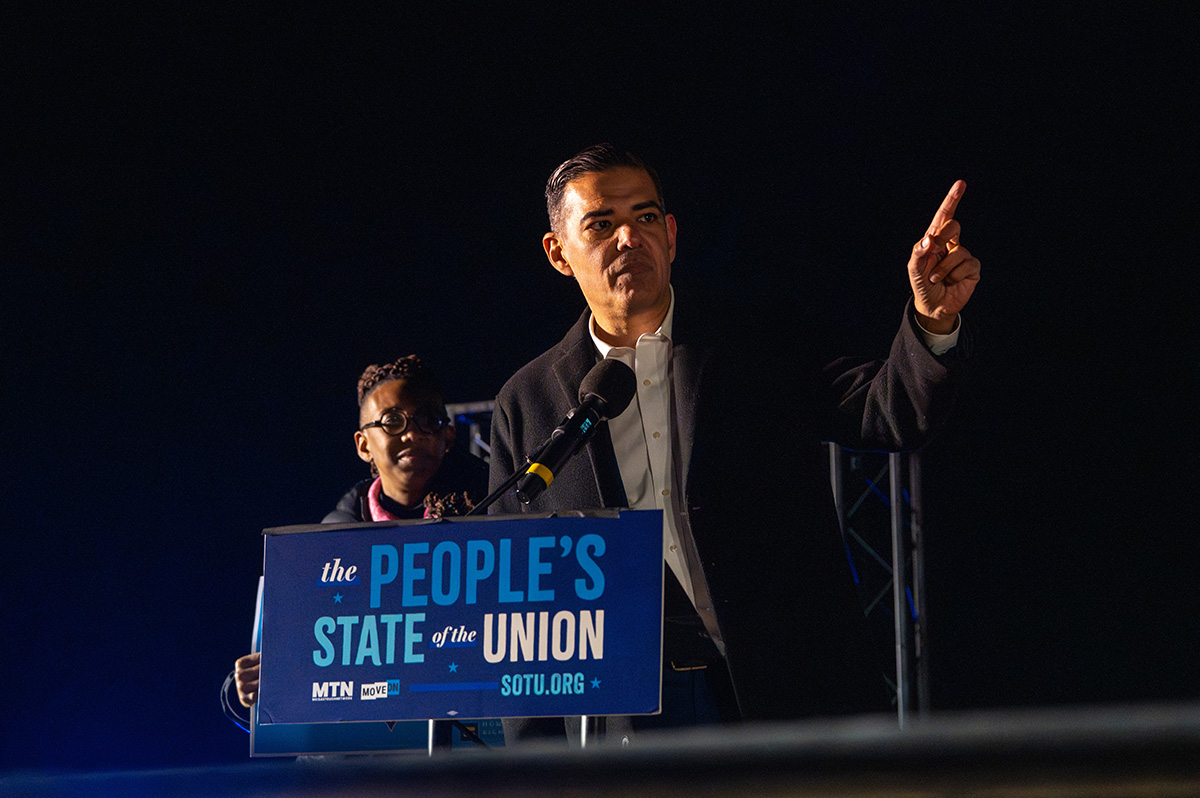
After delivering remarks alongside Robert Garcia, Kelley Robinson, president of the Human Rights Campaign, took the stage and transformed the freezing crowd’s anger into resolve.
Garcia later told the Blade that visibility matters in moments like this — especially when LGBTQ rights are under direct attack.
“We should be crystal clear about right now what is happening in our country,” Garcia said. “We have a president who is leading the single largest government cover up in modern history, we have the single largest sex trafficking ring in modern history right now being covered up by Donald Trump and Pam Bondi In the Department of Justice. Why are we protecting powerful, wealthy men who have abused and raped women and children in this country? Why is our government protecting these men at this very moment? In my place at the Capitol is a woman named Annie farmer. Annie and her sister Maria, both endured horrific abuse by Jeffrey Epstein and Ghislaine Maxwell. As we move forward in this investigation, always center the survivors; we are going to get justice for the survivors. And Donald Trump may call this investigation a hoax. He may try to deflect our work, but our message to him is very clear that our investigation is just getting started, and we will we will get justice for these survivors.”
He told the Blade afterwards that having queer leaders front and center is itself an act of resistance.
“I obviously was very honored to speak with Kelley,” the California representative said. Kelley is doing a great job…it’s important that there are queer voices, trans voices, gay voices, in protest, and I think she’s a great example of that. It’s important to remind the country that the rights of our community continue to be attacked, and then we’ve got to stand up. Got to stand up for this as well.”
Robinson echoed that call, urging LGBTQ Americans — especially young people — not to lose hope despite the administration’s escalating rhetoric.
“There are hundreds of thousands of people that are standing up for you every single day that will not relent and will not give an inch until every member of our community is protected, especially our kids, especially our trans and queer kids. I just hope that the power of millions of voices drowns out that one loud one, because that’s really what I want folks to see at HRC. We’ve got 3.6 million members that are mobilizing to support our community every single day, 75 million equality voters, people that decide who they’re going to vote for based on issues related to our community. Our job is to make sure that all those people stand up so that those kids can see us and hear our voices, because we’re going to be what stands in the way.”
A boycott — and a warning
The list of Democratic lawmakers who boycotted the State of the Union included Sens. Ruben Gallego, Ed Markey, Jeff Merkley, Chris Murphy, Adam Schiff, Tina Smith, and Chris Van Hollen, along with dozens of House members.
For those gathered outside — and for viewers watching the livestream hosted by MoveOn — the counter-programming was not merely symbolic. It was a warning.
While the president spoke of strength and success inside the chamber, LGBTQ Americans — particularly transgender youth — were once again cast as political targets. And outside the Capitol, lawmakers and advocates made clear that the fight over their rights is far from over.
U.S. Military/Pentagon
4th Circuit rules against discharged service members with HIV
Judges overturned lower court ruling

A federal appeals court on Wednesday reversed a lower court ruling that struck down the Pentagon’s ban on people with HIV enlisting in the military.
The conservative three-judge panel on the 4th U.S. Circuit Court of Appeals overturned a 2024 ruling that had declared the Defense Department and Army policies barring all people living with HIV from military service unconstitutional.
The 4th Circuit, which covers Maryland, North Carolina, South Carolina, Virginia, and West Virginia, held that the military has a “rational basis” for maintaining medical standards that categorically exclude people living with HIV from enlisting, even those with undetectable viral loads — meaning their viral levels are so low that they cannot transmit the virus and can perform all duties without health limitations.
This decision could have implications for other federal circuits dealing with HIV discrimination cases, as well as for nationwide military policy.
The case, Wilkins v. Hegseth, was filed in November 2022 by Lambda Legal and other HIV advocacy groups on behalf of three individual plaintiffs who could not enlist or re-enlist based on their HIV status, as well as the organizational plaintiff Minority Veterans of America.
The plaintiffs include a transgender woman who was honorably discharged from the Army for being HIV-positive, a gay man who was in the Georgia National Guard but cannot join the Army, and a cisgender woman who cannot enlist in the Army because she has HIV, along with the advocacy organization Minority Veterans of America.
Isaiah Wilkins, the gay man, was separated from the Army Reserves and disenrolled from the U.S. Military Academy Preparatory School after testing positive for HIV. His legal counsel argued that the military’s policy violates his equal protection rights under the Fifth Amendment’s Due Process Clause.
In August 2024, a U.S. District Court sided with Wilkins, forcing the military to remove the policy barring all people living with HIV from joining the U.S. Armed Services. The court cited that this policy — and ones like it that discriminate based on HIV status — are “irrational, arbitrary, and capricious” and “contribute to the ongoing stigma surrounding HIV-positive individuals while actively hampering the military’s own recruitment goals.”
The Pentagon appealed the decision, seeking to reinstate the ban, and succeeded with Wednesday’s court ruling.
Judge Paul V. Niemeyer, one of the three-judge panel nominated to the 4th Circuit by President George H. W. Bush, wrote in his judicial opinion that the military is “a specialized society separate from civilian society,” and that the military’s “professional judgments in this case [are] reasonably related to its military mission,” and thus “we conclude that the plaintiffs’ claims fail as a matter of law.”
“We are deeply disappointed that the 4th Circuit has chosen to uphold discrimination over medical reality,” said Gregory Nevins, senior counsel and employment fairness project director for Lambda Legal. “Modern science has unequivocally shown that HIV is a chronic, treatable condition. People with undetectable viral loads can deploy anywhere, perform all duties without limitation, and pose no transmission risk to others. This ruling ignores decades of medical advancement and the proven ability of people living with HIV to serve with distinction.”
“As both the 4th Circuit and the district court previously held, deference to the military does not extend to irrational decision-making,” said Scott Schoettes, who argued the case on appeal. “Today, servicemembers living with HIV are performing all kinds of roles in the military and are fully deployable into combat. Denying others the opportunity to join their ranks is just as irrational as the military’s former policy.”
New York
Lawsuit to restore Stonewall Pride flag filed
Lambda Legal, Washington Litigation Group brought case in federal court

Lambda Legal and Washington Litigation Group filed a lawsuit on Tuesday, challenging the Trump-Vance administration’s removal of the Pride flag from the Stonewall National Monument in New York earlier this month.
The suit, filed in the U.S. District Court for the Southern District of New York, asks the court to rule the removal of the Pride flag at the Stonewall National Monument is unconstitutional under the Administrative Procedures Act — and demands it be restored.
The National Park Service issued a memorandum on Jan. 21 restricting the flags that are allowed to fly at National Parks. The directive was signed by Trump-appointed National Park Service Acting Director Jessica Bowron.
“Current Department of the Interior policy provides that the National Park Service may only fly the U.S. flag, Department of the Interior flags, and the Prisoner of War/Missing in Action flag on flagpoles and public display points,” the letter from the National Park Service reads. “The policy allows limited exceptions, permitting non-agency flags when they serve an official purpose.”
That “official purpose” is the grounds on which Lambda Legal and the Washington Litigation Group are hoping a judge will agree with them — that the Pride flag at the Stonewall National Monument, the birthplace of LGBTQ rights movement in the U.S., is justified to fly there.
The plaintiffs include the Gilbert Baker Foundation, Charles Beal, Village Preservation, and Equality New York.
The defendants include Interior Secretary Doug Burgum; Bowron; and Amy Sebring, the Superintendent of Manhattan Sites for the National Park Service.
“The government’s decision is deeply disturbing and is just the latest example of the Trump administration targeting the LGBTQ+ community. The Park Service’s policies permit flying flags that provide historical context at monuments,” said Alexander Kristofcak, a lawyer with the Washington Litigation Group, which is lead counsel for plaintiffs. “That is precisely what the Pride flag does. It provides important context for a monument that honors a watershed moment in LGBTQ+ history. At best, the government misread its regulations. At worst, the government singled out the LGBTQ+ community. Either way, its actions are unlawful.”
“Stonewall is the birthplace of the modern LGBTQ+ rights movement,” said Beal, the president of the Gilbert Baker Foundation. The foundation’s mission is to protect and extend the legacy of Gilbert Baker, the creator of the Pride flag.
“The Pride flag is recognized globally as a symbol of hope and liberation for the LGBTQ+ community, whose efforts and resistance define this monument. Removing it would, in fact, erase its history and the voices Stonewall honors,” Beal added.
The APA was first enacted in 1946 following President Franklin D. Roosevelt’s creation of multiple new government agencies under the New Deal. As these agencies began to find their footing, Congress grew increasingly worried that the expanding powers these autonomous federal agencies possessed might grow too large without regulation.
The 79th Congress passed legislation to minimize the scope of these new agencies — and to give them guardrails for their work. In the APA, there are four outlined goals: 1) to require agencies to keep the public informed of their organization, procedures, and rules; 2) to provide for public participation in the rule-making process, for instance through public commenting; 3) to establish uniform standards for the conduct of formal rule-making and adjudication; and 4) to define the scope of judicial review.
In layman’s terms, the APA was designed “to avoid dictatorship and central planning,” as George Shepherd wrote in the Northwestern Law Review in 1996, explaining its function.
Lambda Legal and the Washington Litigation Group are arguing that not only is the flag justified to fly at the Stonewall National Monument, making the directive obsolete, but also that the National Park Service violated the APA by bypassing the second element outlined in the law.
“The Pride flag at the Stonewall National Monument honors the history of the fight for LGBTQ+ liberation. It is an integral part of the story this site was created to tell,” said Lambda Legal Chief Legal Advocacy Officer Douglas F. Curtis in a statement. “Its removal continues the Trump administration’s disregard for what the law actually requires in their endless campaign to target our community for erasure and we will not let it stand.”
The Washington Blade reached out to the NPS for comment, and received no response.
-

 Mexico4 days ago
Mexico4 days agoUS Embassy in Mexico issues shelter in place order for Puerto Vallarta
-

 Real Estate4 days ago
Real Estate4 days ago2026: prices, pace, and winter weather
-

 Theater4 days ago
Theater4 days agoJosé Zayas brings ‘The House of Bernarda Alba’ to GALA Hispanic Theatre
-

 Netherlands4 days ago
Netherlands4 days agoRob Jetten becomes first gay Dutch prime minister




















