Health
Another study reports PrEP effectiveness
3 of 275 seroconverted on Truvada: researchers


A new study offers more evidence that pre-exposure prophylaxis (PrEP) can be an effective HIV prevention strategy.
NEW YORK — A study published last week offers more evidence that pre-exposure prophylaxis (PrEP) is an effective prevention strategy for keeping sexually active gay men HIV-negative.
Previous studies have shown that Truvada can reduce the risk of HIV infection but it was unclear if the benefits would be offset by an increase in risky behavior. But as British researchers report in the Sept. 9 edition of the Lancet, Truvada is highly effective, U.S. News & World Report and several other outlets report.
A team of researchers led by Sheena McCormack, of the Medical Research Council clinical trials unit at University College London, sought to investigate this issue.
The randomized trial, which was conducted at 13 sexual health clinics in England, involved HIV-negative gay men who had had anal sex at least once without a condom within 90 days.
The researchers randomly assigned 275 of the men to receive Truvada right away. Another 269 men received the treatment after a delay of one year. The researchers conducted a follow-up with the men every three months. The participants and the researchers were aware of their assigned treatment group, U.S. News & World Report reports.
Based on early findings suggesting that PrEP is highly effective, the trial steering committee recommended in October 2014 that all participants in the delayed-treatment group be offered the preventive treatment.
Among the men who received treatment right away, three HIV infections occurred, compared to 20 in the delayed-treatment group, the study found. The researchers calculated those in the immediate-treatment group had an 86 percent relative reduction in their risk for infection with the virus compared to the group that received delayed treatment, U.S. News & World Report reports.
Meanwhile, the prevalence of sexually transmitted infections, such as syphilis, gonorrhea or chlamydia, was similar in both treatment groups.
“This finding is highly encouraging for PrEP implementation, although quantifying the likely demand in the U.K. remains challenging.The impressive reduction in HIV incidence in people taking PrEP, without a measurable increase in other sexually transmitted infections, is reassuring for clinical, community and public health stakeholders,” McCormack and colleagues concluded, according to U.S. News & World Report.
Health
UNAIDS to commemorate Zero Discrimination Day’s 10th anniversary
UN agency urges global action to protect human rights

As the world marks the 10th anniversary of Zero Discrimination Day; UNAIDS is sounding the alarm on the increasing threats to human rights, calling for renewed efforts to protect the rights of all individuals as a fundamental step towards ensuring health for everyone.
Established by UNAIDS a decade ago, Zero Discrimination Day aims to promote equality and fairness regardless of gender, age, sexuality, ethnicity or HIV status. The progress achieved over the past years is now in jeopardy, however, due to rising attacks on the rights of women, LGBTQ people and other marginalized communities.
UNAIDS Executive Director Winnie Byanyima emphasized the critical link between protecting human rights and safeguarding public health.
“The attacks on rights are a threat to freedom and democracy and are harmful to health,” she said in a press release. “Stigma and discrimination obstruct HIV prevention, testing, treatment and care and hold back progress towards ending AIDS by 2030. It is only by protecting everyone’s rights that we can protect everyone’s health.”
Despite challenges, there has been notable progress.
At the onset of the AIDS pandemic more than 40 years ago, two-thirds of countries criminalized consensual same-sex sexual relations. They are now decriminalized in two-thirds of countries. An additional 38 countries around the world have pledged to end HIV-related stigma and discrimination, contributing to positive changes that include 50 million more girls attending school compared to 2015.
To sustain and enhance these advancements; UNAIDS urges global support for women’s rights movements, LGBTQ rights, racial justice, economic justice, climate justice and peace initiatives. By standing with communities advocating for their rights, the U.N. aims to reinforce the collective effort towards a more inclusive and equitable world.
Zero Discrimination Day is observed on March 1.
Events and activities that will take place around the world throughout the month will serve as reminders of the essential lesson and call to action: Protecting everyone’s health is synonymous with protecting everyone’s rights.
“Through upholding rights for all, we will be able to achieve the Sustainable Development Goals and secure a safer, fairer, kinder and happier world — for everyone,” said Byanyima.
Health
New CDC report finds transgender women at higher risk for HIV
More than 1,600 people in seven cities surveyed

The Centers for Disease Control and Prevention issued a new study report this week that revealed that restricted by employment and housing discrimination and lack of access to needed gender-affirming healthcare for transgender women increasing the risk of contracting HIV.
Researchers reviewed data from a 2019-2020 survey, the National HIV Behavioral Surveillance Among Transgender Women, which found that the demographics of HIV/AIDS have been disproportionally high, especially among Black and Latina trans women, who had experienced employment and housing discrimination coupled with lack of access to gender-affirming healthcare.
The Jan. 25 Morbidity and Mortality Weekly Report was based on data studies of more than 1,600 trans women in seven major urban locales. Participants from Atlanta, Los Angeles, New Orleans, New York, Philadelphia, San Francisco and Seattle were chosen by referrals from people and community-based organizations who knew or were part of the local population of trans women.
The study’s researchers noted: “Employment discrimination occurs at the overlapping nexus of poverty, homelessness, incarceration, health insurance, disability, food insecurity and survival sex work. These issues are interconnected.”
The study stated that trans women’s inability to access quality healthcare, including gender-affirming treatment or access to PrEP, and can expose them to potential incarceration as many turn to “survival sex work” and violence, which increases the risk of contracting HIV.
The study’s author’s pointed out: “When economically marginalized transgender women are refused employment, this refusal cyclically contributes to economic hardships. This analysis …demonstrates the importance of transgender women working and living with dignity and without fear of unfair treatment.”
Health
A Whole New Perspective on Well-Being
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.

It’s easy to spot the distinctive, elegant silhouette of The Mather, a Life Plan Community for those 62+ opening this spring in Tysons, Virginia. What is not apparent to the naked eye is The Mather’s unique wellness philosophy, which is literally built into the community.
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.
Nature is one of the important factors that contribute to well-being. So The Mather is incorporating biophilic design—a design approach to facilitate access to nature or things that replicate natural patterns. This can include interior spaces with sightlines to a garden, choosing natural wood and stone as interior materials, or incorporating fragrant flowers and plants indoors to spark memories and provide tactile opportunities such as gardening.

“Providing biophilic design within interior settings connects residents to the natural world,” says Mary Leary, CEO and President of Mather, the organization behind The Mather. “Research shows that a connection to nature provides positive benefits to mental states and overall well-being. At The Mather, biophilic design is the intersection of buildings and programs with nature in an urban setting.”
“The Mather is attracting a diverse group of older adults,” says Mary. “As a result, we aim to incorporate wellness practices from around the world, including Wyda movement theory of the Celtic Druids, which helps people achieve harmony with nature and contentment through mindfulness.” This holistic regenerative approach is similar to Qi Gong and yoga, while born in a different part of the world. Mather Institute has a special focus on mindfulness to support older adults’ practice of present moment awareness, which can lead to increased overall well-being, compassion, and joy.
A very different example of a wellness offering at The Mather is the Gharieni Welnamis spa wave bed, which uses computer-controlled vibrational therapy and audio frequencies to train the brain to relax. “The bed increases mindfulness, concentration, and creativity—all of which support our mission of creating Ways to Age Well,SM” says Mary.
These and other personalized ways to wellness will ensure that residents of The Mather can choose from seemingly countless ways to focus on their well-being. In other words, the sky’s the limit!
-

 Africa2 days ago
Africa2 days agoCongolese lawmaker introduces anti-homosexuality bill
-

 Colorado4 days ago
Colorado4 days agoFive transgender, nonbinary ICE detainees allege mistreatment at Colo. detention center
-

 Politics4 days ago
Politics4 days agoFirst lady warns Trump is ‘dangerous to the LGBTQ community’ at HRC event
-
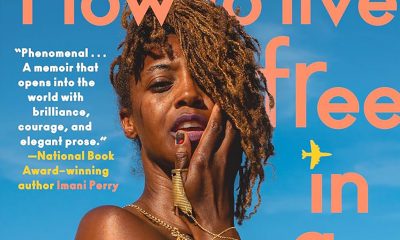
 Books5 days ago
Books5 days agoNew book offers observations on race, beauty, love












