Health
With time, the Monkeypox vaccine provides good protection
In clinical trials, recipients who were HIV negative had an 83 percent immune response 28 days after one dose compared to 98 percent with two doses at 42 days.

A review of academic literature published in the Journal of Internet Medical Research last year determined, when it comes to information about health topics, social media is not the place to turn. (Unless you follow me, of course!) One study found 87 percent of health-related posts contain misinformation. More than 40 percent of posts about vaccines contain incorrect information.
These findings are, perhaps, not surprising. But they are important to keep in mind as we doom-scroll for information about monkeypox.
I’ve already seen a number of posts on Twitter claiming to have monkeypox breakthrough infections after vaccination. One author said they developed a monkeypox rash two weeks after vaccination. While this person’s experience was not likely a breakthrough case, the post brings up important questions. How much protection does a person have after being vaccinated and when? And, as some cities move to a one-dose regimen due to vaccine supply, what does research say about the number of doses needed to protect a person?
Monkeypox rashes and lesions can take up to three weeks to develop after exposure to the virus, which means it is possible the Twitter user mentioned above was exposed before vaccination or shortly after. The time following vaccination and when you are exposed to the virus matters in terms of the amount of protection you have.
Simply put: vaccines do not offer protection immediately after being administered. Remember what we learned when getting our COVID-19 vaccines: no matter which vaccine you received, you were not fully protected until two weeks after the final dose. For the monkeypox vaccine the time to protection is actually longer. Clinical trials indicated it takes up to four weeks for patients to develop strong protection. In fact, two weeks after the first dose, the immune response was just 29 percent! Take extra care during this period to prevent spread.
Now, what about one dose versus two? With limited monkeypox vaccine supply, cities and states should consider limiting doses to one per person to protect more people.
The U.S. Food and Drug Administration (FDA) approved a vaccine, Jynneos, developed by the U.S. government and Bavarian Nordic in 2019 to protect against both monkeypox and smallpox. The FDA recommended a two dose regimen, four weeks apart. This regimen outperformed an older smallpox vaccine (ACAM2000) for producing an immunological response. The Jynneos vaccine also has fewer side effects and is much safer.
Unfortunately, the Jynneos vaccine is in very short supply. Bavarian Nordic, the only manufacturer of the vaccine worldwide, says it can produce 30 million doses of Jynneos annually, meaning with a full regimen less than 15 million patients worldwide will have full protection. That’s why cities like Washington, D.C. and New York have chosen to move to a single-dose regimen. The United Kingdom and some countries in Europe have done the same.
This approach is the right one.
In clinical trials, recipients who were HIV negative had an 83 percent immune response 28 days after one dose compared to 98 percent with two doses at 42 days. HIV positive recipients had a 67 percent immune response 28 days after one dose. It was 96 percent 42 days after two doses.
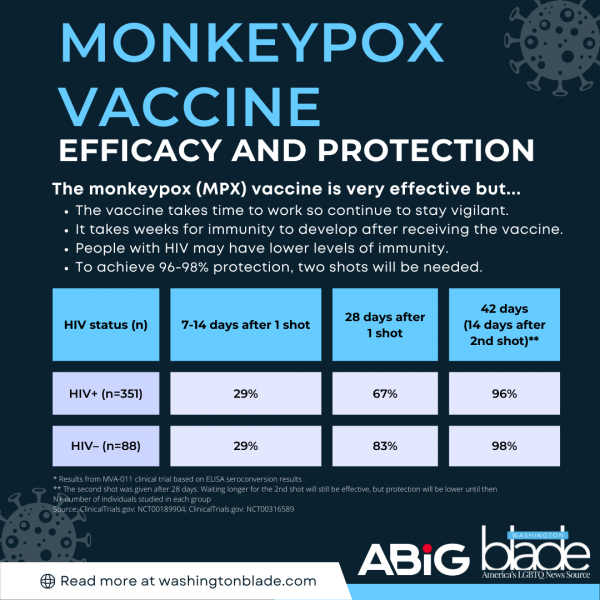
While that data indicates a two-dose regimen is best, with supplies limited, a one-dose regimen for most people is a reasonable approach. That strategy allows double the group of individuals to be immunized — even though there is slightly lower efficacy. A recent article in Science highlighted this important point. Jynneos’ CEO, an immunologist, said one dose of the vaccine conferred a “robust immune response.”
There is one caveat, however. Based on the clinical trial data, we might need to stick with the original two-dose regimen for people who are immunocompromised or live with HIV (irrespective of immune status).
In the face of what appears to be a public health system in disarray, Americans need to be partners in fighting the virus’ spread. Get vaccinated when available. Individuals who are most at risk should sign up now to receive a vaccine. Second, understand it takes time after receiving the vaccine to develop immunity whether you are HIV positive or not. Understand monkeypox symptoms, the timing of symptoms and how to reduce your risk. And, of course, take care when it comes to social media. Spread truth.
Dr. N. Adam Brown is a practicing emergency medicine physician, founder of a healthcare strategy advisory group ABIG Health, and a professor of practice at the University of North Carolina’s Kenan-Flagler Business School. Previously he served as President of Emergency Medicine and Chief Impact Officer for a leading national medical group. Follow him on Twitter @ERDocBrown.
Health
UNAIDS to commemorate Zero Discrimination Day’s 10th anniversary
UN agency urges global action to protect human rights

As the world marks the 10th anniversary of Zero Discrimination Day; UNAIDS is sounding the alarm on the increasing threats to human rights, calling for renewed efforts to protect the rights of all individuals as a fundamental step towards ensuring health for everyone.
Established by UNAIDS a decade ago, Zero Discrimination Day aims to promote equality and fairness regardless of gender, age, sexuality, ethnicity or HIV status. The progress achieved over the past years is now in jeopardy, however, due to rising attacks on the rights of women, LGBTQ people and other marginalized communities.
UNAIDS Executive Director Winnie Byanyima emphasized the critical link between protecting human rights and safeguarding public health.
“The attacks on rights are a threat to freedom and democracy and are harmful to health,” she said in a press release. “Stigma and discrimination obstruct HIV prevention, testing, treatment and care and hold back progress towards ending AIDS by 2030. It is only by protecting everyone’s rights that we can protect everyone’s health.”
Despite challenges, there has been notable progress.
At the onset of the AIDS pandemic more than 40 years ago, two-thirds of countries criminalized consensual same-sex sexual relations. They are now decriminalized in two-thirds of countries. An additional 38 countries around the world have pledged to end HIV-related stigma and discrimination, contributing to positive changes that include 50 million more girls attending school compared to 2015.
To sustain and enhance these advancements; UNAIDS urges global support for women’s rights movements, LGBTQ rights, racial justice, economic justice, climate justice and peace initiatives. By standing with communities advocating for their rights, the U.N. aims to reinforce the collective effort towards a more inclusive and equitable world.
Zero Discrimination Day is observed on March 1.
Events and activities that will take place around the world throughout the month will serve as reminders of the essential lesson and call to action: Protecting everyone’s health is synonymous with protecting everyone’s rights.
“Through upholding rights for all, we will be able to achieve the Sustainable Development Goals and secure a safer, fairer, kinder and happier world — for everyone,” said Byanyima.
Health
New CDC report finds transgender women at higher risk for HIV
More than 1,600 people in seven cities surveyed

The Centers for Disease Control and Prevention issued a new study report this week that revealed that restricted by employment and housing discrimination and lack of access to needed gender-affirming healthcare for transgender women increasing the risk of contracting HIV.
Researchers reviewed data from a 2019-2020 survey, the National HIV Behavioral Surveillance Among Transgender Women, which found that the demographics of HIV/AIDS have been disproportionally high, especially among Black and Latina trans women, who had experienced employment and housing discrimination coupled with lack of access to gender-affirming healthcare.
The Jan. 25 Morbidity and Mortality Weekly Report was based on data studies of more than 1,600 trans women in seven major urban locales. Participants from Atlanta, Los Angeles, New Orleans, New York, Philadelphia, San Francisco and Seattle were chosen by referrals from people and community-based organizations who knew or were part of the local population of trans women.
The study’s researchers noted: “Employment discrimination occurs at the overlapping nexus of poverty, homelessness, incarceration, health insurance, disability, food insecurity and survival sex work. These issues are interconnected.”
The study stated that trans women’s inability to access quality healthcare, including gender-affirming treatment or access to PrEP, and can expose them to potential incarceration as many turn to “survival sex work” and violence, which increases the risk of contracting HIV.
The study’s author’s pointed out: “When economically marginalized transgender women are refused employment, this refusal cyclically contributes to economic hardships. This analysis …demonstrates the importance of transgender women working and living with dignity and without fear of unfair treatment.”
Health
A Whole New Perspective on Well-Being
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.

It’s easy to spot the distinctive, elegant silhouette of The Mather, a Life Plan Community for those 62+ opening this spring in Tysons, Virginia. What is not apparent to the naked eye is The Mather’s unique wellness philosophy, which is literally built into the community.
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.
Nature is one of the important factors that contribute to well-being. So The Mather is incorporating biophilic design—a design approach to facilitate access to nature or things that replicate natural patterns. This can include interior spaces with sightlines to a garden, choosing natural wood and stone as interior materials, or incorporating fragrant flowers and plants indoors to spark memories and provide tactile opportunities such as gardening.

“Providing biophilic design within interior settings connects residents to the natural world,” says Mary Leary, CEO and President of Mather, the organization behind The Mather. “Research shows that a connection to nature provides positive benefits to mental states and overall well-being. At The Mather, biophilic design is the intersection of buildings and programs with nature in an urban setting.”
“The Mather is attracting a diverse group of older adults,” says Mary. “As a result, we aim to incorporate wellness practices from around the world, including Wyda movement theory of the Celtic Druids, which helps people achieve harmony with nature and contentment through mindfulness.” This holistic regenerative approach is similar to Qi Gong and yoga, while born in a different part of the world. Mather Institute has a special focus on mindfulness to support older adults’ practice of present moment awareness, which can lead to increased overall well-being, compassion, and joy.
A very different example of a wellness offering at The Mather is the Gharieni Welnamis spa wave bed, which uses computer-controlled vibrational therapy and audio frequencies to train the brain to relax. “The bed increases mindfulness, concentration, and creativity—all of which support our mission of creating Ways to Age Well,SM” says Mary.
These and other personalized ways to wellness will ensure that residents of The Mather can choose from seemingly countless ways to focus on their well-being. In other words, the sky’s the limit!
-

 State Department2 days ago
State Department2 days agoState Department releases annual human rights report
-

 Maryland4 days ago
Maryland4 days agoJoe Vogel campaign holds ‘Big Gay Canvass Kickoff’
-

 Autos5 days ago
Autos5 days agoSport haulers: Jeep Grand Cherokee, Mercedes GLE-Class
-

 Politics3 days ago
Politics3 days agoSmithsonian staff concerned about future of LGBTQ programming amid GOP scrutiny












