Health
The graying of AIDS: living longer with HIV
‘None of us expected to live this long’
D.C. resident John Klenert signed up for a National Institutes of Health-funded AIDS study at Johns Hopkins University in 1984. The Centers for Disease Control reported the first cases of what became known as AIDS three years earlier, but some of Klenert’s friends had already passed away from the virus by the time the research project had begun.
“We figured if there was going to be a cure that we would be the first ones to volunteer to get these tests,” he said.
Johns Hopkins researchers in 1986 screened the first blood samples that Klenert and other study participants had given once scientists discovered the virus that causes AIDS. “For me, the first blood I had given was positive,” he said. “I would have been shocked had I turned out to be negative.”
Older people with HIV will be the focus of a July 25 forum at the International AIDS Conference. Panelists will include Ricardo Jimenez of the Ecuadorian Red Cross, Carolyn Massey of Older Women Embracing Life, Inc., Wojciech Tomczynski of the Polish Network of People Living with HIV/AIDS Association and Ruth Waryaro of Help Age International in Uganda. Doctor Kevin Fenton of the Centers for Disease Control and Prevention and Stephen Karpiak and Mark Brennan-Ing of AIDS Community Research Initiative of America’s Center on HIV and Aging and New York University College of Nursing are among those who are scheduled to speak during the plenary.
The CDC estimates that 10.8 percent of the roughly 50,000 new HIV infections that occur each year in the United States are among those older than 50. It further reports that 16.7 percent of new diagnoses in 2009 were among this demographic, with half of them also having AIDS. Federal health officials predict that half of people with HIV in the United States by 2015 will be older than 50.
ACRIA, the New York-based Gay Men’s Health Crisis and Services and Advocacy for GLBT Elders co-organized the forum as part of what SAGE Senior Director of Public Policy Robert Espinoza described to the Blade as a need to increase visibility around HIV-related aging issues.
“We feel it’s an important conversation because there are so many people who are aging with HIV and AIDS,” he told the Blade.
Increased access to treatment in the United States and other developed countries has allowed more people with HIV to live longer. The arrival of more widely available anti-retroviral drugs in the mid-1990s has also contributed to this trend.
“If you were 35 in 1990 and you made it to the mid to late 90s and got on protease inhibitors, there’s a good chance you’re still alive today and you’d be above 50,” said ACRIA executive director Daniel Tietz. “And that’s the reality.”
Older people with HIV face unique challenges
Johns Hopkins and CDC researchers noted earlier this year that older people with HIV are more likely to suffer higher rates of cardiovascular disease, osteoporosis, non-AIDS related cancers and other chronic illnesses. Klenert, who is now 63, has had a brain tumor removed and an operation to repair an aneurysm over the last 30 years. He said that his neurologist and cardiologist both said that his HIV status did not contribute to either of these conditions.
“There are many folks who age into this — they’ve had HIV for a while, their HIV is reasonably well-managed,” said Tietz. “It’s their other things. It’s their hypertension, the diabetes, the heart disease that are posing challenges in terms of management.”
This population also faces the same hurdles that service providers maintain older LGBT people without the virus routinely face. These include a lack of health care, financial insecurity and social isolation, but a person’s HIV status can acerbate these problems.
“The LGBT community in general is not great on aging issues; they tend to be more youth centered,” said Espinoza. “We find that a lot of older adults with HIV are often looking just for both the caregiving support they need to manage their health and remain optimistic and maintain their emotional health, but they are looking for community.”
He and other service providers stressed that stigmas associated with HIV and sexuality can dissuade older people from discussing their sexual health with doctors and other health care providers.
“If you’re not talking openly to people who manage your health then it’s going to then prevent the kind of services you need to age successfully,” said Espinoza, further stressing that many health care providers don’t even provide HIV tests to their older patients who could have just become sexually active after leaving a relationship or getting divorced. “We’re dealing with constituents who have been living with HIV and AIDS for years. We’re dealing with constituents who have been infected for years, but just got diagnosed, which often means the illness has progressed more in their bodies. And then we’re also dealing with constituents who just became infected and are trying to assimilate to both the emotional and health issues related to their infection.”
The New York City Council has funded ACRIA’s efforts to bolster HIV prevention efforts among older New Yorkers with HIV. The National Institutes of Health’s Office of AIDS Research has also established a working group to study the virus’ impact on older people.
“I don’t think government officials have put this on their radar screen as much as they should,” said Espinoza. “As the demographic really begins growing in the next two years, we’re going to see more questions from aging providers and health care professionals about what it means to appropriately serve older adults with HIV and engage them in their facilities or in their long-term care facilities. And with that, I’m hoping that government officials will also increase their attention and increase the funding for that kind of programmatic prevention.”
Seeking to increase visibility
Those who advocate on behalf of older people with HIV further stress that lack of visibility remains a problem.
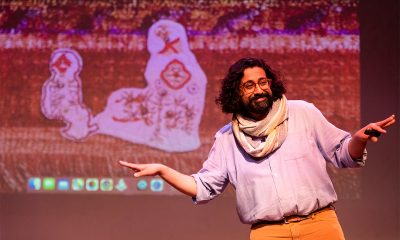
The Graying of AIDS project profiles older people with the virus as a follow-up to photojournalist Katja Heinemann’s eponymous photo essay that “Time” published in 2006 to mark the epidemic’s 25th anniversary. D.C. resident Ronald Johnson, vice president of policy and advocacy for AIDS United, is among the 11 people that Heinemann and Naomi Schegloff profile in photographs and short videos.
Schegloff, who works in the public health field, told the Blade that she “very much appreciated” what she described as “frank discussions” about sexuality that took place with many of those whom she and Heinemann profiled. Discrimination, a desire for companionship and a general lack of information about HIV are also common themes.
“A lot of older adults have not been on the market in the last 30 years, or have barely been on the market in the last 30 years,” said Schegloff. “If they’ve been with a partner — married or otherwise — for a long time, they may or may not have dated at a time when HIV was something we knew about. If for them condoms are something that you use to avoid getting pregnant and they’re heterosexual and they’re a woman and they’ve gone through menopause, they’re not worried about that anymore. And it used to be that for people of a certain generation, the worst thing you could get through sex as one person told us in an interview is something you can take penicillin for now. They weren’t necessarily thinking about this thing [HIV] as being relevant to them.”
Heinemann and Schegloff plan to photograph and interview those from the United States and around the world who are interested in participating in their project during the Global Village at the International AIDS Conference. They will upload images, interview excerpts and other content to an online exhibition during the five-day gathering.
“For us as a visual project and a documentary project, we’re hoping to really put a face to this that will be a little bit of a wakeup call where you don’t just read the statistic,” said Heinemann. “But you’re also able to see oh yeah wait a minute, this is not just Bill in Chicago and Ronald in D.C. This is also a person from Tanzania; this is also a person from Russia or someone from India.”
Klenert, a former Victory Fund and Gay and Lesbian Alliance Against Defamation board member, also reflected upon those with HIV who continue to grow older.
“I’d like to think that people in my age group are hopeful as well as surprised,” he said in response to a question about the changes he has seen since he tested positive. “I’m guessing that most of us didn’t think that we would live this long. There’s that old greeting card [that says] had I lived this long I would have taken better care of us. Back when we were in our 30s — or late 30s — none of us expected to live this long because back then the mortality rate was almost 100 percent.”
Health
UNAIDS to commemorate Zero Discrimination Day’s 10th anniversary
UN agency urges global action to protect human rights

As the world marks the 10th anniversary of Zero Discrimination Day; UNAIDS is sounding the alarm on the increasing threats to human rights, calling for renewed efforts to protect the rights of all individuals as a fundamental step towards ensuring health for everyone.
Established by UNAIDS a decade ago, Zero Discrimination Day aims to promote equality and fairness regardless of gender, age, sexuality, ethnicity or HIV status. The progress achieved over the past years is now in jeopardy, however, due to rising attacks on the rights of women, LGBTQ people and other marginalized communities.
UNAIDS Executive Director Winnie Byanyima emphasized the critical link between protecting human rights and safeguarding public health.
“The attacks on rights are a threat to freedom and democracy and are harmful to health,” she said in a press release. “Stigma and discrimination obstruct HIV prevention, testing, treatment and care and hold back progress towards ending AIDS by 2030. It is only by protecting everyone’s rights that we can protect everyone’s health.”
Despite challenges, there has been notable progress.
At the onset of the AIDS pandemic more than 40 years ago, two-thirds of countries criminalized consensual same-sex sexual relations. They are now decriminalized in two-thirds of countries. An additional 38 countries around the world have pledged to end HIV-related stigma and discrimination, contributing to positive changes that include 50 million more girls attending school compared to 2015.
To sustain and enhance these advancements; UNAIDS urges global support for women’s rights movements, LGBTQ rights, racial justice, economic justice, climate justice and peace initiatives. By standing with communities advocating for their rights, the U.N. aims to reinforce the collective effort towards a more inclusive and equitable world.
Zero Discrimination Day is observed on March 1.
Events and activities that will take place around the world throughout the month will serve as reminders of the essential lesson and call to action: Protecting everyone’s health is synonymous with protecting everyone’s rights.
“Through upholding rights for all, we will be able to achieve the Sustainable Development Goals and secure a safer, fairer, kinder and happier world — for everyone,” said Byanyima.
Health
New CDC report finds transgender women at higher risk for HIV
More than 1,600 people in seven cities surveyed

The Centers for Disease Control and Prevention issued a new study report this week that revealed that restricted by employment and housing discrimination and lack of access to needed gender-affirming healthcare for transgender women increasing the risk of contracting HIV.
Researchers reviewed data from a 2019-2020 survey, the National HIV Behavioral Surveillance Among Transgender Women, which found that the demographics of HIV/AIDS have been disproportionally high, especially among Black and Latina trans women, who had experienced employment and housing discrimination coupled with lack of access to gender-affirming healthcare.
The Jan. 25 Morbidity and Mortality Weekly Report was based on data studies of more than 1,600 trans women in seven major urban locales. Participants from Atlanta, Los Angeles, New Orleans, New York, Philadelphia, San Francisco and Seattle were chosen by referrals from people and community-based organizations who knew or were part of the local population of trans women.
The study’s researchers noted: “Employment discrimination occurs at the overlapping nexus of poverty, homelessness, incarceration, health insurance, disability, food insecurity and survival sex work. These issues are interconnected.”
The study stated that trans women’s inability to access quality healthcare, including gender-affirming treatment or access to PrEP, and can expose them to potential incarceration as many turn to “survival sex work” and violence, which increases the risk of contracting HIV.
The study’s author’s pointed out: “When economically marginalized transgender women are refused employment, this refusal cyclically contributes to economic hardships. This analysis …demonstrates the importance of transgender women working and living with dignity and without fear of unfair treatment.”
Health
A Whole New Perspective on Well-Being
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.

It’s easy to spot the distinctive, elegant silhouette of The Mather, a Life Plan Community for those 62+ opening this spring in Tysons, Virginia. What is not apparent to the naked eye is The Mather’s unique wellness philosophy, which is literally built into the community.
The Mather’s team recognizes that everyone’s wellness journey is completely unique to their life experiences and influences.
Nature is one of the important factors that contribute to well-being. So The Mather is incorporating biophilic design—a design approach to facilitate access to nature or things that replicate natural patterns. This can include interior spaces with sightlines to a garden, choosing natural wood and stone as interior materials, or incorporating fragrant flowers and plants indoors to spark memories and provide tactile opportunities such as gardening.

“Providing biophilic design within interior settings connects residents to the natural world,” says Mary Leary, CEO and President of Mather, the organization behind The Mather. “Research shows that a connection to nature provides positive benefits to mental states and overall well-being. At The Mather, biophilic design is the intersection of buildings and programs with nature in an urban setting.”
“The Mather is attracting a diverse group of older adults,” says Mary. “As a result, we aim to incorporate wellness practices from around the world, including Wyda movement theory of the Celtic Druids, which helps people achieve harmony with nature and contentment through mindfulness.” This holistic regenerative approach is similar to Qi Gong and yoga, while born in a different part of the world. Mather Institute has a special focus on mindfulness to support older adults’ practice of present moment awareness, which can lead to increased overall well-being, compassion, and joy.
A very different example of a wellness offering at The Mather is the Gharieni Welnamis spa wave bed, which uses computer-controlled vibrational therapy and audio frequencies to train the brain to relax. “The bed increases mindfulness, concentration, and creativity—all of which support our mission of creating Ways to Age Well,SM” says Mary.
These and other personalized ways to wellness will ensure that residents of The Mather can choose from seemingly countless ways to focus on their well-being. In other words, the sky’s the limit!